We asked students with chronic illness what helped them in their journey.
How Gender-Affirming Hormone Therapy Affects Chronic Disease
How Gender-Affirming Hormone Therapy Affects Chronic Disease
Here’s what LGBTQ+ patients and allies need to know about how this life-saving therapy can impact underlying conditions.
June 18, 2024
Kelsey Kloss
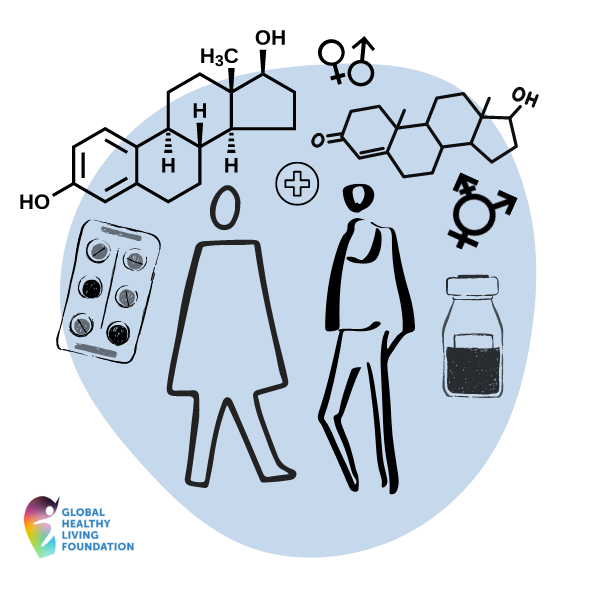
Although hormone therapy can be used to treat menopause or certain cancers, it’s also used to help transgender patients as part of a gender transition.
In this case, it’s typically called gender-affirming hormone therapy, and it consists of either feminizing (estrogen) or masculinizing (testosterone) hormones to help patients’ bodies reflect their gender identity, per Planned Parenthood.
Although not all transgender people choose to or are able to transition medically, socially, or financially, gender-affirming hormone therapy is a key part of transitioning for many of them.
Transitioning is the process of aligning with your gender identity rather than the sex assigned at birth. It can help improve mental health and overall well-being by helping transgender people feel happier with their appearance.
Many transgender people choose to take hormones indefinitely, so it’s particularly important to consider underlying conditions and overall health impacts.
“You want to be sure your chronic health issues are being managed as you are transitioning, because now it’s another process that your body is going through,” says Julius Joi Johnson-Weaver, MD, a Black, neurodivergent, trans, nonbinary physician.
For Grayson Schultz, a transmasculine sex educator, it was difficult to find data on hormone therapy and its potential implications on his Still’s disease (a rare type of inflammatory arthritis) when he started taking testosterone in 2020.
“I tried to find journal articles about any of the medications for Still’s disease and patients starting hormone replacement therapy,” says Schultz. “But, unsurprisingly, I found nothing. Providers had no anecdotal data, either.”
This lack of data not only impacted his mental health, but almost prevented him from getting hormone replacement therapy at all.
“I was honestly a little terrified that somehow hormone replacement therapy might affect the efficacy of one of the only few FDA-approved medications for my condition,” says Schultz. “I navigated multiple panic attacks over this and almost didn’t start testosterone at all.”
Impact of Hormone Therapy on Chronic Disease
The role hormone therapy plays on chronic disease in transgender people is complex and under-researched. Although more studies are needed to cover a wide range of chronic diseases in those receiving gender-affirming care, here’s what we know about the relationship between hormone therapy and certain conditions in transgender people.
Understanding the Benefits
“Hormones are used all the time in therapeutic ways for cisgender individuals, whether it’s to help improve chronic pain, sexual function, or the effects of aging,” says Schultz. “But these methods aren’t being gatekept in the same way as hormone replacement therapy for transgender people.”
Mental Health
Studies show that hormone therapy can improve mental health outcomes for transgender individuals. Gender-affirming hormone therapy was consistently found to reduce depressive symptoms and psychological distress in transgender people in a 2023 review published in Nature Human Behaviour.
Transgender people experience mental health problems like depression, anxiety, and social isolation at far greater rates than the general population, per the review.
Although it’s uncertain if hormone therapy benefits mental health due to chemical changes in the brain, improved self-image, or both, it’s clear that it can help reduce depressive symptoms and improve psychosocial functioning in transgender individuals.
Chronic Pain
Although very few studies have looked at changes in pain perception and pain-related conditions in transgender people, research has consistently shown variances in pain perception based on testosterone or estrogen levels.
Testosterone appears to have protective factors in biological males and in transgender males receiving testosterone hormone replacement, while estrogen fluctuations may play a role in lower pain threshold, per a 2023 review in the International Journal of Molecular Sciences.
For instance, feminizing hormone therapy tends to increase pain such as headache and musculoskeletal pain, while testosterone hormone therapy tends to decrease it.
“One amazing positive for me in starting testosterone is that it has helped immensely with my chronic pain, especially from hypermobile Ehlers-Danlos Syndrome (hEDS),” says Schultz. “There hasn’t yet been much research on this, but it seems to happen nearly across the board from what I’ve seen in other hEDSers on testosterone.”
Large, long-term studies are still needed to determine the best approach for treatment and prevention of pain in transgender individuals, especially when it comes to gender-affirming medical interventions and related medical care, note the authors of a 2024 review in Frontiers in Pain Research.
Bone Health
Sex steroids, particularly estrogen, play an important role in attaining and maintaining peak bone density in all people, per a 2019 review in Clinical Reviews in Bone and Mineral Metabolism.
Many studies show that pharmacologic estrogen may improve bone density in transgender women, while bone density in transgender men remains largely unchanged with pharmacologic testosterone.
Potential Risk Factors
Despite the numerous benefits, hormone therapy can potentially enhance or create risk factors related to some chronic health conditions that need careful consideration. It is best to speak with your doctor to make sure your chronic disease(s) and any medications you take currently are in full consideration when thinking about beginning hormone therapy.
Cardiovascular Health
Those who take hormone replacements as part of gender-affirming therapy have a higher risk of serious cardiac events such as stroke, heart attack, and pulmonary embolism, according to research presented at the 2023 Annual Scientific Session Together With the World Congress of Cardiology hosted by the American College of Cardiology.
In particular, researchers examined heart-related events in more than 21,000 people with gender dysphoria (the condition in which a person’s gender identity doesn’t match the sex they were assigned at birth), of whom 1,675 had used hormone replacement therapy.
Those who had ever used hormone replacements had nearly seven times the risk of ischemic stroke, nearly six times the risk of ST elevation myocardial infarction (the most serious heart attack type), and nearly five times the risk of pulmonary embolism (a lung artery blockage) compared with those who had never used it.
Both estrogen and testosterone have been shown to increase blood clotting, which could explain the higher risk of these clotting-related heart events, according to the researchers. However, hormone replacement therapy was not associated with an increase in deaths from any cause or higher rates of atrial fibrillation, diabetes, hypertension, hemorrhagic stroke, or heart failure.
“Starting transitioning is a big part of a person’s life and helping them feel more themselves, but hormone replacement therapy also has a lot of side effects — it’s not a risk-free endeavor,” said study author Ibrahim Ahmed, MD, in a statement. “Looking at a person’s medical and family history should definitely be part of the screening protocol before they even start hormone replacement therapy.”
Metabolic Health
Hormone therapy may have different metabolic impacts on transgender men and women.
For instance, testosterone therapy in transgender men has been found to increase lean mass, decrease fat mass, and have no impact on insulin resistance, while evidence in transgender women shows that feminizing hormone therapy may have the opposite effects, per a 2020 review in the World Journal of Diabetes.
However, other research shows that weight gain during hormone therapy may be a concern for both transmasculine and transfeminine individuals. Transmasculine individuals had greater rates of obesity and weight gain before and during hormone therapy compared with transfeminine individuals, according to a 2021 study in the International Journal of Obesity.
After 11 to 21 months of hormone therapy, weight gain of about 11 pounds or more was seen in 21 percent of transfeminine individuals and 30 percent of transmasculine individuals.
The prevalence of diabetes in transgender people undergoing sex hormone therapy is also mixed, since many studies only ask binary gender (male/female questions), per a 2021 study in Clinical Diabetes.
“Health care providers should attempt to reduce diabetes and cardiovascular risk factors among all people, with a particular attention to transgender patients taking hormone therapies,” note the study authors.
More research is needed to fully understand the impact of gender-affirming hormone therapy on body composition and insulin resistance.
Despite some existing research on hormone therapy and bone health, there are still many unknowns when it comes to how it impacts certain conditions.
Specific Considerations for Nonbinary Individuals
Similar to transgender men and women, nonbinary people can also see immense benefits from access to hormones — including an improved quality of life, better mental health, and decreased gender dysphoria and suicidality, per the University of Melbourne.
Nonbinary is a broad term for those whose gender does not fit into the woman or man gender binary specifically. In recent years, there has been improved access to gender-affirming hormone therapy for nonbinary patients.
Previously, these patients often had to pretend they were transgender to access what was needed, since many doctors would not provide alternative doses of hormone therapy to nonbinary individuals. However, a 2024 University of Melbourne survey of 271 nonbinary Australians found that 66 percent had used or wanted hormone therapy.
Still, there is a lack of data on efficacy and safety on hormone treatment in nonbinary individuals and there are currently no evidence-based protocols for standardized hormone treatment in these patients, per a 2020 review in the Journal of Clinical Medicine.
More research is needed, and clinicians may need to combine different hormonal formulations to respond to specific requests from nonbinary patients.
The Role That Providers Play
Health care providers, of course, also play an integral role in delivering comprehensive care. It’s important to feel comfortable speaking with your provider about all aspects of your health, including any existing chronic conditions or the desire for gender-affirming hormone therapy.
Currently, the process of gender-affirming care differs by state and clinics due to differences in state laws, but generally, transgender patients can start by visiting a health care provider that specializes in this care.
Some patients may be referred to a specialized clinic or provider after talking about their gender dysphoria to a primary care provider or therapist.
Directories such as the World Professional Association for Transgender Health (WPATH), the LGBTQ+ Healthcare Directory, and Outcare Health can help you find gender-affirming care.
For medical specialists, the National LGBTQIA+ Health Education Center from The Fenway Institute also provides free continuing education for mental health providers, primary care providers, and some subspecialties. The National Center for Transgender Equality also provides free resources for transgender people and others on rights related to health insurance, health care and more.
Over time, better provider training may make conversations with your primary physician easier.
“Access is still the biggest obstacle,” says Dr. Johnson-Weaver. “We need more people who are offering it, meaning providers are trained well. Primary care providers can provide hormone care — people do not need to go to specialists for this, it just needs to be in our rubric.”
Initially for Schultz, his primary care provider was a leader in transgender health care in his community and was able to provide the most help. “My other providers — rheumatologist, allergist, neurologist, and so forth — weren’t very familiar with transgender health care, even as it overlapped with their areas of expertise,” says Schultz.
However, after moving from Wisconsin to Ohio, he’s now seeing a provider at Planned Parenthood for hormones.
“With the difficulties in finding providers locally that are covered by insurance and knowledgeable about trans health, I’ll probably continue to get my hormones there,” says Schultz. “I’m not looking forward to likely having to find a primary care provider 45 to 70 minutes away from my rural city. But I’m grateful that I can at least access hormones where I live.”
Dr. Johnson-Weaver adds that better provider training and education could eventually help with the cost of transitioning, another barrier to access. This training begins as early as medical school for providers.
“Improving access and well-rounded doctors who are not biased against the queer and trans community is going to go a long way,” says Dr. Johnson-Weaver. “I am seeing medical schools doing more of that, which could be helpful in the long run.”
Creating Change for LGBTQ+ IBD
At the Global Healthy Living Foundation, we recognize the unique health challenges faced by the LGBTQ+ community, including those living with IBD. That’s why we launched our “LGBTQ+ IBD experiences” survey centered on capturing and understanding your experiences.
Through the community voices from our survey, we uncovered insights on everything from confronting health disparities in IBD care to navigating inclusivity in health care settings. We hope that these findings can now help inform and educate both the community and health care professionals, to ensure you receive better access to care and improved condition management. Check out the report now!
Sources:
Gender-Affirming Care. Planned Parenthood. Accessed June 20, 2024. https://www.plannedparenthood.org/planned-parenthood-great-northwest-hawaii-alaska-indiana-kentuck/patients/health-care-services/hrt-hormone-therapy-for-trans-and-non-binary-patients.
Interview with Julius Joi Johnson-Weaver, MD, a Black, neurodivergent, trans, non-binary physician
Hormone Therapy for Gender Dysphoria May Raise Cardiovascular Risks. American College of Cardiology. February 23, 2023. https://www.acc.org/About-ACC/Press-Releases/2023/02/22/20/29/Hormone-Therapy-for-Gender-Dysphoria-May-Raise-Cardiovascular-Risks.
Spanos C, et al. Effects of gender-affirming hormone therapy on insulin resistance and body composition in transgender individuals: A systematic review. World Journal of Diabetes. March 15, 2020. doi: https://doi.org/10.4239/wjd.v11.i3.66.
Kyinn M, et al. Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. International Journal of Obesity. August 16, 2021. doi: https://doi.org/10.1038/s41366-021-00935-x.
Moverley J, et al. Considerations for Transgender People With Diabetes. Clinical Diabetes. October 2021. doi: https://doi.org/10.2337/cd21-0011.
Rothman MS, et al. Bone Health in the Transgender Population. Clinical Reviews in Bone and Mineral Metabolism. July 2, 2019. doi: https://doi.org/10.1007/s12018-019-09261-3.
Transgender (trans) people and osteoporosis. Royal Osteoporosis Society. December 2021. https://theros.org.uk/information-and-support/osteoporosis/causes/transgender-trans-people-and-osteoporosis/.
Interview with Grayson Schultz, a transmasculine sex educator.
Doyle DM, et al. A systematic review of psychosocial functioning changes after gender-affirming hormone therapy among transgender people. Nature Human Behaviour. May 22, 2023. doi: https://doi.org/10.1038/s41562-023-01605-w.
Athnaiel O, et al. The Role of Sex Hormones in Pain-Related Conditions. International Journal of Molecular Sciences. January 18. 2023. doi: https://doi.org/10.3390/ijms24031866.
Anger JT, et al. Pain mechanisms in the transgender individual: a review. Frontiers in Pain Research. March 27, 2024. doi: https://doi.org/10.3389/fpain.2024.1241015.
Non-Binary People Have Hormone Therapy and Surgery More Often Than You Might Think. The University of Melbourne. March 26, 2024. https://pursuit.unimelb.edu.au/articles/non-binary-people-have-hormone-therapy-and-surgery-more-often-than-you-might-think.
Cocchetti C, et al. Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals. Journal of Clinical Medicine. May 26, 2020. doi: https://doi.org/10.3390/jcm9061609.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo







