In honor of World IBD Day, dietitians from three different continents share tips on managing diet and inflammatory bowel disease (IBD).
10 THINGS YOU SHOULD NEVER SAY TO SOMEONE WITH CROHN’S DISEASE OR ULCERATIVE COLITIS
10 THINGS YOU SHOULD NEVER SAY TO SOMEONE WITH CROHN’S DISEASE OR ULCERATIVE COLITIS
November 30, 2020
Kelsey Kloss
If you live with a chronic illness, you know how difficult it can be to explain your condition to others. This may be especially true if you look healthy and your condition is largely invisible, like Crohn’s disease or ulcerative colitis tend to.
However, these two forms of inflammatory bowel disease (IBD) can be debilitating and might even lead to life-threatening complications, per the Mayo Clinic. Ulcerative colitis causes long-term inflammation and sores (or ulcers) in the innermost lining of the colon and rectum, while Crohn’s disease can cause inflammation anywhere in the lining of your digestive tract, which often spreads far into affected tissues.
These conditions may cause a wide range of symptoms, including severe diarrhea, bloody stool, abdominal pain and cramping, reduced appetite, fatigue, and unintended weight loss. People with inflammatory disease often require immunosuppressive medication to reduce inflammation in the digestive tract and control symptoms.
IBD shouldn’t be confused with irritable bowel syndrome (IBS), which affects the large intestine and can cause cramping, bloating, and a change in bowel habits. While IBS causes discomfort, it doesn’t cause inflammation and damage to the intestines, per the U.S. National Library of Medicine.
People with IBD may face uncomfortable or unintentionally hurtful questions from loved ones, acquaintances, and even complete strangers. While you might mean well when chatting with someone who has IBD, it can be easy to say something that comes across the wrong way.
“A lot of people underestimate the severity of inflammatory bowel disease, and I think it’s because patients who have it don’t necessarily have outward symptoms,” says Christine Bishara, MD, an internist with a focus on gut health and wellness medicine in New York City.
Here are 10 things you should avoid saying to someone who has inflammatory bowel disease, with some background on why they might hit the wrong note.
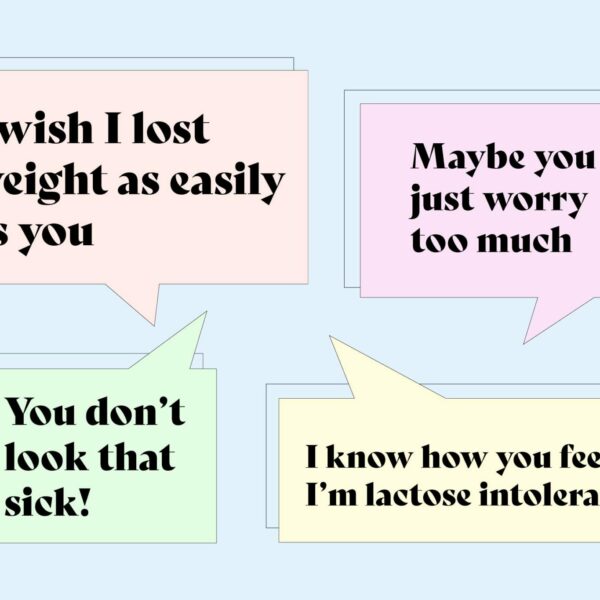
1. “I wish I lost weight as easily as you.”
This may be a tempting statement to make if you try to highlight the positive, but many patients with Crohn’s or ulcerative colitis don’t intentionally try to lose weight. They may have a poor appetite, issues with absorbing nutrients from food, or simply can’t tolerate most foods at times, and might even need to resort to liquid oral supplementation to get their nutrition, according to UCSF Health.
“I have a family member with Crohn’s disease, and someone said to her, ‘I wish I could have diarrhea all day as well so I could stay skinny,’” says Dr. Bishara. “But these patients frequently lose weight because they are nutritionally depleted from not being able to absorb nutrients due to inflammation.”
Commenting about weight loss or eating habits in general can also come off as suspicious or judgemental. Samantha R. is a 23-year-old in Los Angeles who works in marketing for the online pharmacy Honeybee Health, and she experienced that suspicion when she was diagnosed with ulcerative colitis at age 21.
“There have been periods where I couldn’t eat anything, and some people made comments that I was too concerned with losing weight or following a fad diet if I wasn’t eating at a meal,” she says. “It was really frustrating, because all I wanted was to be able to eat a normal meal, feel like I was full, and not throw up from it.”
On the other hand, corticosteroids like prednisone are anti-inflammatory drugs often prescribed to those with IBD that can cause someone to put on pounds.
“Prednisone is notorious for causing weight gain,” says Dr. Bishara. “It can cause your face to look a little bloated and full, like a moon-shaped face. People will comment on that and say, ‘Oh, your face looks chubbier!’ but it’s really a side effect of the medications the patient is on.”
In short: If you’re talking to someone with Crohn’s disease or ulcerative colitis, there’s no need to mention their weight unless they want to speak about it.
2. “You’re tired again today? Let’s go grab coffee!”
The fatigue that those with chronic illnesses like IBD face is very different from the way other people feel tired after a bad night’s sleep or staying up too late.
“At my worst, when I hadn’t yet managed my ulcerative colitis with medication, I had what felt like two hours of being awake each day before I was really struggling to push through the rest,” says Samantha. “It’s really difficult to explain fatigue to people who haven’t experienced it, and to describe what it feels like when your body is shutting down.”
People with IBD may need to rest often, which others may mistakenly interpret as being lazy or skirting responsibilities.
“There was definitely a misconception that I was being lazy or that I wasn’t self-disciplined enough if I was napping instead of working,” says Samantha R. “Even when people like my professors were really understanding, it was hard for me to ask for accommodations. I had my own self-judgment and felt like I wasn’t trying hard enough.”
3. “C’mon, don’t be antisocial!”
On that note, fatigue and other symptoms may cause someone with IBD to skip out on social gatherings. People might feel uncomfortable going out if they know they can’t eat or they’re worried about access to a bathroom. Try not to question their reasons for staying home.
“I’m not being anti-social, I’m not being lazy, and I’m not a buzzkill,” says Samantha. “That was a stigma I faced as my friends were adjusting to the fact that I had this condition. I simply could not act like others my age, who were going to parties or pulling all-nighters for classes.”
Plus, the person with IBD may already feel down about missing an event without added pressure from friends and family.
“A lot of people would tell me, ‘Why are you acting so old?’” says Samantha. “That was frustrating to deal with because I already felt like I was missing out on a lot. I was already beating myself up for not pushing through more, especially before my diagnosis when I didn’t know what was happening.”
4. “Maybe you just worry too much.”
Up to 40 percent of patients with IBD experience abnormal levels of anxiety, according to a 2015 review in the journal Clinical and Experimental Gastroenterology. IBD disease activity is closely linked to psychological symptoms like anxiety, which tends to be observed more during flares of IBD patients.
This may be one reason other people often blame IBD symptoms on anxiety. However, these are two distinct and different conditions.
“I’ve had anxiety for a long time, so when I first started having ulcerative colitis symptoms, they were often dismissed as me just being anxious,” says Samantha R. “I dealt with symptoms for four months longer than I needed to because everyone told me I was being anxious. I started believing that and dismissed my symptoms as made-up, when they were 100 percent not.”
While stress and anxiety can contribute to flares of inflammatory bowel disease, they do not cause it.
5. “You should really try to go all-natural.”
Someone’s treatment plan is very specific to them and the severity of their IBD — and it’s a conversation that should be reserved for them and their doctor.
“Some people have really mild IBD that resolves with dietary measures, while others need immune-modulating medications,” says Dr. Bishara.
Try not to give unsolicited advice on someone’s treatment plan because they’ve likely already discussed several options with their doctors.
“I work at a pharmacy and I still have people telling me I’m poisoning my body with prescription medications, when it’s the only thing that got me into remission,” says Samantha.
6. “You’re still having those symptoms?”
Although treatment can help Crohn’s and colitis patients reach remission and avoid relapses for their best quality of life, there is no cure for IBD, according to the University of Chicago Medicine. Symptoms can come and go and it’s common to have long periods of “normal” health with periodic (and highly disruptive) flares.
“I was able to get into remission after a year of medication, but it’s hard to explain to people — especially those my age who usually don’t have long-term health problems — that this is something I’m going to have to take into account for the rest of my life,” says Samantha.
IBD patients often weigh the choices they make with potential outcomes, even if they seem well or aren’t experiencing symptoms.
“Every decision I make takes into account whether or not something could be too much stress for my body and push me out of remission,” says Samantha R. “I’m constantly having to make these calculations and cost-benefit analyses.”
7. “How did you get it?”
The exact cause of IBD is still unknown. While stress and diet were previously suspected, experts now know that these factors might aggravate IBD but don’t cause it, according to the Mayo Clinic. Genetics or an abnormal immune system response to an invading virus or bacterium could play a role, but more research is needed.
“I think the majority of the population doesn’t know what having IBD means from a histological point of view, and many people probably just think, ‘Oh, whatever, they have a sensitive stomach,’” says Dr. Bishara. “When really, you’re having an inflammatory response.”
Asking someone what caused their IBD can make them feel as though they did something to bring it upon themselves, which is never the case.
“Someone might say, ‘It’s because you were anxious all those years,’ or ‘You didn’t eat healthy enough,’” says Samantha R. “There’s a lot of judgment there. Trust me, the person with the diagnosis is already judging themselves, because they suddenly have very different capabilities than what they’re used to.”
8. “You don’t look that sick!”
While IBD doesn’t always lead to visible symptoms, it can cause serious complications.
“A lot of times people don’t think patients with IBD are as sick as they really are,” says Dr. Bishara. “I’ve had patients who needed to be hospitalized for dehydration and other severe symptoms, even if they don’t necessarily look that sick.”
Depending on how well you know the person you’re speaking to, they may be willing to explain some of their symptoms to you. However, be careful about how you approach the topic, because some statements can come off as accusatory.
“You can be sympathetic and say, ‘I’m so sorry to hear that — can you tell me a little more about your symptoms?’” says Dr. Bishara. “I would say the majority of patients are happy to explain that, but perhaps not when they’re approached in a manner that’s suspicious or accusatory of the fact that they don’t look sick.”
9. “I know how you feel — I’m lactose intolerant.”
You may be trying to relate, but even two people with IBD may have completely different experiences from one another, let alone two people with different gastrointestinal conditions.
“Someone with lactose intolerance has a completely different reason for having diarrhea than someone who has IBD,” says Dr. Bishara. The same is true for people with irritable bowel syndrome (IBS) or other gastrointestinal digestive issues.
When you’re lactose intolerant, you’re unable to fully digest the sugar (lactose) in milk and may experience diarrhea, gas, and bloating after consuming dairy products. Although it’s uncomfortable, it’s usually harmless and can be treated with a low-lactose diet, per the Mayo Clinic.
Whether you have a lactose intolerance or are sensitive to another food, try not to compare your condition to someone else’s.
10. “My cousin’s friend cured herself with chamomile tea!”
People with IBD have heard about remedy after remedy from others, but they’ve likely already tried several treatment options.
“The severity of the disease varies between individuals, so what might work for one person might not necessarily work for another,” says Dr. Bishara. “People can feel like you’re trying to tell them they must not be doing the right thing if you give them unsolicited advice.”
It’s also important to keep in mind that while certain lifestyle habits might help reduce the inflammation that triggers symptoms, there is no magical cure for IBD.
“I can’t tell you how many times people have told me ‘I think you’re just not drinking enough water’ or ‘If you only meditated for five minutes every day, you wouldn’t have any of these symptoms,’” says Samantha. “People also tell me autoimmune conditions can be cured with the right all-natural diet, which is just scientifically wrong.”
What’s more, someone with IBD has likely already put a lot of time, energy, and effort into feeling better, and unsolicited recommendations can seem dismissive of that.
“There’s this assumption that I’m not doing everything I can,” says Samantha R. “It’s almost a little bit of judgment, as though I’m not trying hard enough to fix my ulcerative colitis. But I assure you, I don’t want to be dealing with this either.”
Banana AS, et al. Inflammatory bowel disease and anxiety: links, risks, and challenges faced. Clinical and Experimental Gastroenterology. March 23, 2015. doi: www.doi.org/10.2147/CEG.S57982.
Inflammatory bowel disease (IBD). Mayo Clinic. March 3, 2020. https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315.
Inflammatory Bowel Disease (IBD) Treatment. UChicagoMedicine. October 27, 2020. https://www.uchicagomedicine.org/conditions-services/inflammatory-bowel-disease/treatment.
Interview with Christine Bishara, MD, an internist with a focus on gut health and wellness medicine in New York City
Lactose Intolerance. Mayo Clinic. April 7, 2020. https://www.mayoclinic.org/diseases-conditions/lactose-intolerance/symptoms-causes/syc-20374232.
Nutrition Tips for Inflammatory Bowel Disease. UCSF Health. October 27, 2020. https://www.ucsfhealth.org/education/nutrition-tips-for-inflammatory-bowel-disease.
U.S. National Library of Medicine. Irritable Bowel Syndrome. October 27, 2020. https://medlineplus.gov/irritablebowelsyndrome.html.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo