Accessing the right asthma treatment isn't always easy. Understand common treatment barriers and get tips to enhance your asthma care.
Navigating Asthma Care and Comorbid Conditions with Confidence
Navigating Asthma Care and Comorbid Conditions with Confidence
Take charge of your asthma and associated conditions. Get insider tips on teaming up with specialists and confidently advocating for the best care possible
September 26, 2023
Nina Wasserman

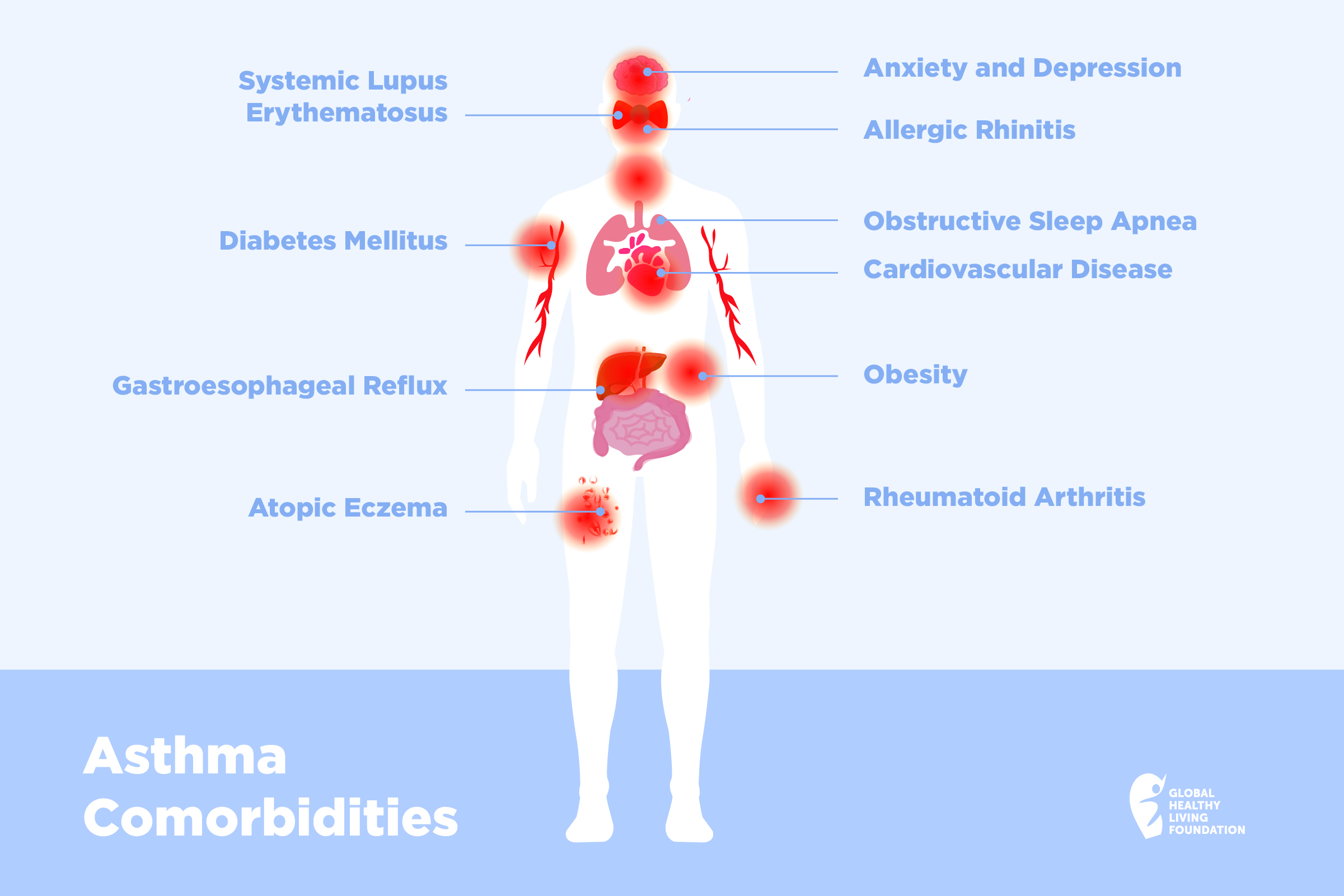
If you have asthma, chances are you also experience related comorbidities. An asthma comorbidity is any additional condition that can affect people with asthma.
These conditions could affect your sleep, eating habits, activity, and overall emotional well-being. Sometimes, these conditions can actually make your asthma worse or make it harder to treat. It’s important to talk to your specialist about overlapping/co-occurring conditions in order to be able to treat them comprehensively.
Prevalence of Comorbidities in Asthma Patients
Asthma is associated with a high prevalence of comorbidities. These conditions impact the whole body — they are not just related to the respiratory system.
A 2020 study published in Nature found that 54 percent of adults with asthma reported having one or more non-respiratory comorbid conditions.
The most common respiratory comorbidity for asthma is allergic rhinitis, says Barbara Yawn, MD, MSc, FAAFP, Adjunct Professor at the University of Minnesota. In fact, asthma is found in 38 percent of people with allergic rhinitis and nasal symptoms are present in up to 85 percent of people with asthma, according to a 2022 study in the journal Scientific Reports.
Because rhinitis blocks the airways, it’s important to get it treated. “People might just say it’s a stuffy nose, but if it’s not under control, your asthma may not get under control,” says Dr. Yawn.
People with asthma are also twice as likely to have gut and urinary conditions — and about 50 percent more likely to have obesity or hypertension.
Other conditions linked to asthma include:
- Atopic eczema, a condition that causes dry, flaky skin
- Obstructive sleep apnea (OSA), a sleep-related breathing disorder
- Gastroesophageal reflux (GERD), when stomach acid flows back into the esophagus
- Anxiety and depression, the latter can make it more difficult to focus on using your asthma medications making both the asthma and the depression worse
Also, people with asthma are almost twice as likely to have a cardiovascular condition, compared to people without asthma, and have a 60 percent higher chance of cerebrovascular conditions, according to studies. Recently, shingles has been added to the list, according to Dr. Yawn.
Smoking and/or vaping should also be considered a comorbidity of asthma, says Dr. Yawn. “Smoking is a tobacco addiction and it is therefore a disease, which absolutely has to be treated,” she says. “Get help for smoking cessation.” If you have asthma, it’s time to kick the habit.
If your asthma is not properly treated and managed, you have a higher chance of experiencing comorbidities. That’s why it’s really important to have good communication with your doctor about your asthma symptoms.
Why You Should Treat Other Health Issues Along with Asthma
Other health problems can make asthma worse, as shown in the Nature study. So, it’s important to find and treat any other health issues you have at the same time as your asthma.
But, figuring out these problems can be hard. Some health issues have the same symptoms as asthma. This can make it confusing to know what’s really going on. Asthma has similar symptoms to the following conditions:
- Vocal cord dysfunction symptoms include chest tightness and wheezing.
- Obstructive sleep apnea can cause shortness of breath upon waking, as the airways become blocked during sleep. A proper sleep study can tell you if you are waking with asthma or OSA.
- Gastroesophageal reflux can be triggered by certain foods and may cause wheezing or coughing.
- Obesity can cause breathlessness.
After you know for sure what other health problems you have, treating them can make your asthma better. This means when you treat one problem, it can help with another.
Here are a few examples:
- Rhinitis: If you have rhinitis and you treat it with special nose sprays, you’re less likely to need emergency care for asthma.
- Obesity: If you get your asthma under better control, you are able to do more activity, which can help your fitness, says Dr. Yawn, noting that a different type of asthma, called an non-eosinophilic phenotype, can affect people with obesity and may require a slightly different treatment. If you are overweight and cannot get your asthma under control, talk to a clinician about getting tested for this type of asthma.
- Anxiety or Depression: If your asthma is not under control, your risk of anxiety or depression is even higher. Tell your doctor if you are experiencing emotions of fear, panic or anxiety related to your asthma.
Medications used to treat other conditions can also have a negative impact on your asthma and vice versa, which is why communication with your doctor is essential. For example, beta blockers prescribed for cardiovascular disease or anxiety can cause a tightening of the airways. Asthma therapies can aggravate your GERD.
6 Tips to Communicate with Your Provider About Your Conditions and Treatment Options
We’ve all been there: You wait months for an appointment, only to feel rushed during the actual visit. To prevent leaving the doctor’s office with feelings of dissatisfaction, here are six strategies to maximize the limited time you have with your physician:
Bring Relevant Medical Records/Dates
Have you been to the ER? Consulted a specialist? Walk-in clinics don’t always share records. Keep a record of these dates and bring relevant papers. Note all your current medicines and doses. Dr. Yawn recommends bringing all your medications and inhalers.
Prepare Your Questions
Wondering about medication effectiveness or side effects? Need clarity on certain symptoms? Write down all your questions; it’s easy to forget when time is short.
Share Symptoms, Not Diagnoses
The internet is a great resource, but it’s not a medical degree. Use what you learn online to formulate questions, but avoid self-diagnosing. If online searches have worried you, share this with your doctor. Don’t wait for them to ask — sharing what you feel is vital.
Stay on Topic
With limited time, focus on your main concerns. Briefly describe your symptoms, their frequency, and whether they’re improving or worsening. Decide beforehand what’s most important to discuss.
Be Honest
Are you taking your medicine as prescribed? Following recommended lifestyle changes? If not, be open about it. There are many reasons someone might skip a dose — cost, complicated schedules, or fear of side effects. Honesty ensures your doctor knows how best to help.
Access Medical Information Online
Many medical details — test results, treatments, medications, and more — are available online. After your visit, you’ll likely receive an email to access your profile. Being proactive here can improve communication with your doctor. If you have issues accessing your patient portal, seek assistance.
Getting Your Care Network to Communicate
To manage comorbidities linked to asthma, you might need to consult specialists beyond your primary care doctor. A pulmonologist can treat your asthma, while allergists are also specialists for asthma-related issues.
For associated comorbid conditions, ensure you communicate with the necessary specialists for appropriate treatment and asthma control. Your care team may also include a gastroenterologist for digestive concerns, a cardiologist for heart issues, or an ear, nose, and throat specialist for respiratory complications.
Carly H., who has lupus and has also been dealing with long COVID alongside her asthma, shares her experience of managing multiple specialists for different conditions. “For me, the easiest way is to see specialists from the same hospital network,” she says. “This helps with record sharing and with communication between members of your care team.” Listen to Carly’s story on “The Asthma Podcast.”
Being proactive in her care, Carly emphasizes the importance of clear communication and preparation. “Express clearly that you’d like for the new specialist to work closely with your established physician/team,” she says. “If not, and you have the ability, the next step is to find a physician open to collaborating for your greatest health outcomes.”
Approaching Specialists About Your Comorbidities
Navigating a cohesive approach among various health care professionals can be challenging, yet it’s crucial for your well-being. Here are some strategies to foster collaboration:
Be Politely Persistent
You know your symptoms better than anyone else. It’s vital to let your doctors know if treatments are helping or not. If something a doctor says doesn’t feel right to you, speak up and share your feelings. Always trust your instincts when it comes to your health.
Get Them Up to Speed
To make sure everyone’s on the same page with your care, always bring your meds with you to appointments. It’s also a good idea to print out a quick summary of your visits to share with your main doctor and any specialists. Most importantly, speak up and look out for yourself – make sure your health needs get the attention they deserve.
Re-Evaluate
If your symptoms are not going away, or getting worse for no apparent reason, it’s worth going back to your doctor to see if you have developed a new comorbidity or one that has yet to be detected.
Be Confident and Ask
It may be time for a second opinion. You may feel uncomfortable, like you are going behind our doctor’s back, but it’s really not a big deal from their standpoint. Their goal should be to get you the best care.
It’s important to stay ahead of all your conditions and understand that they can be interrelated.
“Simply put, you never know how one is impacting the other,” says Carly. “Treating one illness often is helpful in managing the other. For example, oftentimes treating my lupus and the inflammation associated with it, is integral to keeping my asthma under control because my lupus disease activity often manifests in my lungs.”
The bottom line: You are your best advocate in getting your medical team to work together to get you the best asthma care.
Acevedo-Prado, A, et al. Association of rhinitis with asthma prevalence and severity. Scientific Reports. April 16, 2022. doi: https://doi.org/10.1038/s41598-022-10448-w.
Interview with Barbara Yawn, MD, MSc, FAAFP, Adjunct Professor at the University of Minnesota.
Kaplan, A, et al. Impact of comorbid conditions on asthmatic adults and children. Nature. August 20, 2020. https://www.nature.com/articles/s41533-020-00194-9.
Su, X, et al. Prevalence of Comorbidities in Asthma and Nonasthma Patients. Medicine. May 2016. doi: https://doi.org/10.1097/MD.0000000000003459.
If you enjoyed reading this article, you’ll love what our video has to offer.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo