Take charge of your asthma and associated conditions. Get tips on teaming up with specialists and confidently advocating for your care.
Understanding Asthma Complications
Understanding Asthma Complications
February 13, 2023
Nina Wasserman
Check out “Our Guide to Personalizing Your Asthma Care” for more information on this topic.
You have to cut your exercise session short because you’re struggling to breathe. Your friend just got a cat, not realizing it means you can’t visit their home anymore. Yet another scenario: You’re outside enjoying a beautiful walk and you get hit with a high pollen count that triggers wheezing.
Having asthma can make daily life challenging, especially if you don’t have it under control, and it can be even more challenging if you’re also dealing with another chronic illness.
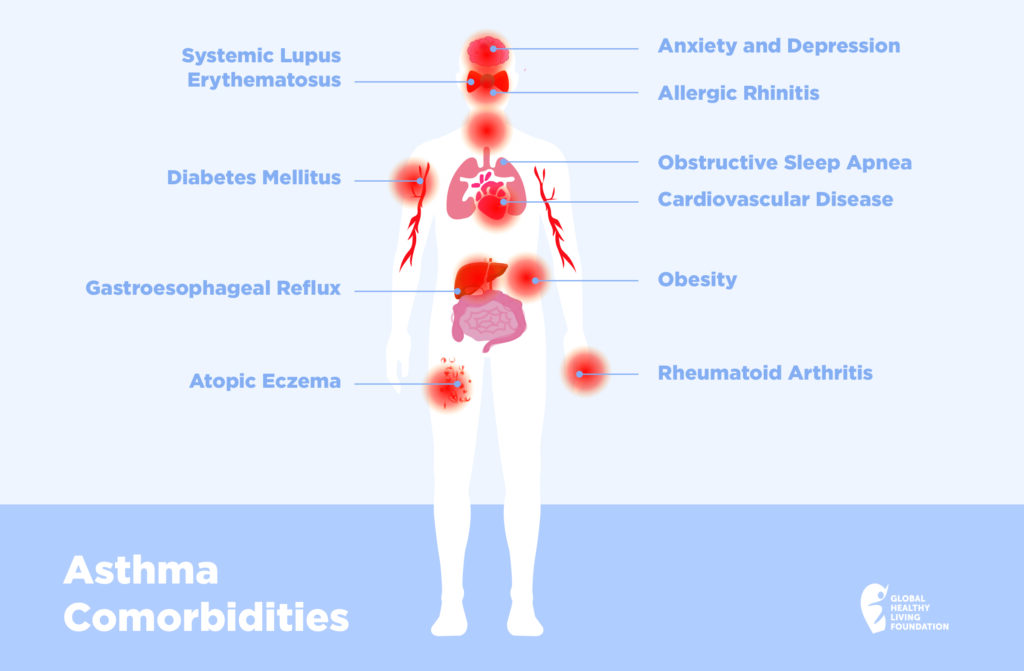
Unfortunately, having asthma can put you at higher risk of other illnesses, or comorbidities, especially in the case of severe asthma. Without proper treatment, you can get stuck in a vicious cycle, as these additional illnesses can actually make your asthma worse.
While it’s still unknown why why asthma is associated with a host of other conditions, we do know that the inflammation caused by asthma is linked to multiple comorbidities.
10 Conditions Linked to Asthma
Here are 10 chronic conditions that are known to be associated with asthma. By educating yourself and taking action, you can tip the odds of staying healthy in your favor.
Allergic Rhinitis
Allergic rhinitis is an inflammation of the nasal passageways caused by allergens such as dust, pollen, mold, or pet dander. It’s a very common condition for people with asthma.
According to a 2022 review published in the Polish Archives of Internal Medicine on recent advances in asthma and its comorbidities, allergic rhinitis was present in 55 percent of people with severe asthma and 60 percent of those with non-severe asthma.
One of the reasons these conditions so often occur together is that asthma and allergic rhinitis share similar allergen triggers and have similar inflammatory pathways. The respiratory tract is continuous from the nasal passages to the lung, making irritation of one likely to irritate the rest of the tract, explains. Dr. Barbara P Yawn, MD, MSc, FAAFP, Adjunct Professor at the University of Minnesota.
Other upper respiratory conditions that are associated with asthma include chronic rhinosinusitis, a swelling of the lining of the sinuses, and nasal polyposis, according to the Polish review.
Chronic rhinosinusitis can increase asthma exacerbations. In those with severe asthma, medical treatment or surgery to improve the rhinosinusitis can improve asthma management. Several new treatments are available for this chronic debilitating condition including biologic medications that are also used for asthma management, says Dr. Yawn. “It is often necessary to control or treat existing allergic rhinitis or chronic rhinosinusitis to achieve good asthma control.”
Atopic Eczema
Atopic eczema is a condition that causes dry, flaky, itchy skin. The symptoms, which can also include oozing, crusting, and swelling, can appear anywhere on the body. People with this chronic condition are at risk of developing asthma, according to the American Academy of Allergy, Asthma and Immunology. Atopic eczema is also associated with food allergies and allergic rhinitis, another condition associated with asthma.
Atopic eczema and asthma have something in common: they can both disrupt sleep. That’s why it’s important to moisturize regularly to soothe the skin and relieve itching. A good skin regimen can also help prevent new outbreaks. If these simple therapies are not enough, some therapies like biologic medicines can treat uncontrolled or severe atopic eczema, according to Dr. Yawn.
Obesity
Obesity is a common comorbidity for people with asthma. While the connection is still being researched, current studies show that the inflammation connected to obesity may contribute to airway inflammation, decreased lung function, and asthma exacerbation.
Research also showed that the more overweight someone is the greater their likelihood is for having asthma. It can be a vicious cycle for people who have asthma that is not well controlled because they may find activity or exercise difficult. This can lead to more weight gain and add to the difficulty of losing weight. Sleep trouble and medication side effects may also play a role, so it’s important to discuss all of these risk factors with your doctor.
Anxiety and Depression
Anxiety affects half of people with severe asthma, compared to 30 percent of people with other chronic respiratory illnesses, reports the Polish review. It’s a vicious cycle: Anxiety can make an asthma attack worse and depression can decrease a person’s motivation to take their asthma medication.
It’s important to talk with your health care professional about symptoms of anxiety and depression so you can work together to develop a treatment plan that might include mindfulness techniques, taking prescription medications, and see a psychotherapist.
Obstructive Sleep Apnea
Along with obesity, obstructive sleep apnea (OSA) and gastroesophageal reflux (GERD) occur at higher rates among those with asthma, according to a 2021 study. Obstructive sleep apnea is a sleep related breathing disorder that occurs when the muscles that support the soft tissues of the throat, like the tongue, temporarily relax, resulting in a blocking of the airway.
If you have both asthma and sleep apnea, it’s important to seek treatment for both conditions.
Gastroesophageal Reflux
Gastroesophageal reflux happens when the stomach acid repeatedly flows back into the esophagus, irritating the lining. Treating reflux can help improve asthma control, says Dr. Yawn.
While obesity, OSA, and GERD all share risk factors, the 2021 study also found they shared inflammatory pathways. They also have the potential to worsen asthma’s symptoms.
Diabetes Mellitus
There is a strong connection between asthma and type 2 diabetes mellitus in women, with nearly double the risk, according to the Polish review. There is also a correlation between the severity of diabetes and reduced lung function.
Obesity may play some role in this increased risk, according to Dr. Yawn, but both diabetes and asthma are conditions of a disrupted immune system.
Cardiovascular Disease
People with asthma have a 42 percent higher risk of cardiovascular disease compared to those without asthma, according to the Polish review. Among those, people with asthma and allergies have an elevated risk of coronary heart disease.
While the connection is still not fully understood, data shows that the systemic inflammation from asthma may impair cardiovascular function.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic inflammatory condition that affects the joints, causing pain, stiffness, swelling and, in some cases, loss of function. It is an autoimmune disease, which means the immune system attacks healthy cells in your body by mistake, causing inflammation.
A 2020 study found a significant relationship between asthma and rheumatoid arthritis, suggesting that people with asthma are more likely to develop RA.
With RA, you can go for periods without experiencing symptoms, called remission. Then there are times when symptoms get worse, known as flares. Exercise can help improve RA symptoms, so it’s important to get the right treatment for your asthma, especially if it’s exercise-induced.
There is a long menu of possible treatments for RA and, according to Dr. Yawn, it’s important to begin RA treatment early rather than simply observing before beginning therapy.
Systemic Lupus Erythematosus
Patients with asthma have a higher risk of systemic lupus erythematosus (SLE), according to a 2021 study in the journal Clinical Rheumatology. SLE is an uncommon autoimmune disease in which the immune system attacks its own tissues, causing tissue damage in the organs.
Affected areas include the joints, skin, brain, lungs, kidneys, and blood vessels. People with SLE experience fatigue, skin rashes, fever and pain or swelling in the joints. While the likelihood of developing SLE or other forms of lupus is low, those with widespread symptoms should be evaluated for lupus and begin treatment immediately if they are diagnosed with it.
Long COVID-19
Some people who have been infected with the virus that causes COVID-19 can experience symptoms long after they recover from infection. They may be known as COVID long-haulers, but the medical term is Post Acute Sequelae of COVID-19 (PASC).
While initially there was thought to be a link between asthma and COVID-19, new research is showing differently. One recent study found that people with asthma are not at any greater risk for long COVID than those without asthma.
According to the Allergy Asthma Network, about 10 to 30 percent of people infected with COVID-19 experience some long term symptoms. In addition to shortness of breath, symptoms can include:
- Coughing
- Debilitating fatigue
- Body aches
- Joint pain
- Shortness of breath
- Loss of taste or smell (even if this did not occur during the illness)
- Difficulty sleeping
- Headaches
- Muscle weakness
- Nausea
- Anxiety or depression or other mental health symptoms (even in those without a prior history)
- Brain fog
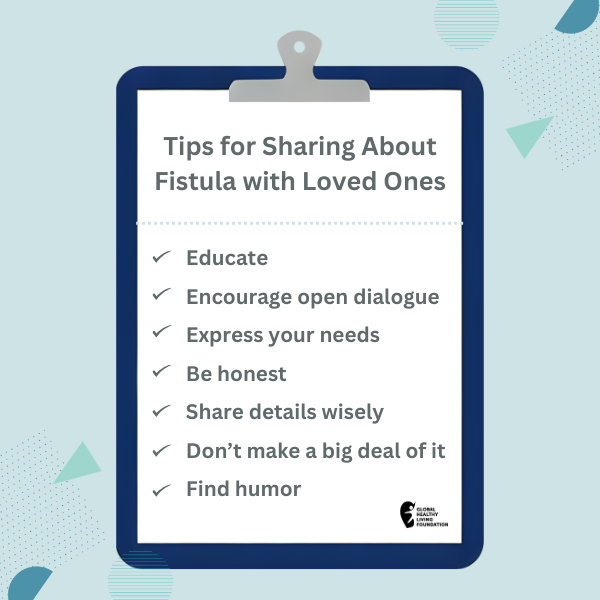
Talking to Your Partner
Carly H, a member of the LGBTQ+ community, has asthma and lupus. She says the key to managing both illnesses has been open and honest communication with her partner. “You need to express exactly what is going on and not leave them guessing,” she says. “It took a while for me to get to that point. I don’t like to ask for help.”
Dealing with chronic illness can be hard. It can also make you feel alone, even when you are not. Here are some tips to foster your relationship in the midst of your illness.
- Be honest; don’t lie about your symptoms. If you feel lousy, say so.
- Give your partner a chance to care for you — you may feel like a burden, but they likely want to help.
- Express your needs and feelings with being critical or endlessly complaining.
- Allow yourself space; it’s okay to take some time for yourself.
- Remain intimate, meaning spend quality time together.
- Be open about your expectations, but accept your partner’s boundaries
- Don’t feel guilty if you can’t do certain things. Your partner should know your limitations and so should you.
Talking to Your Medical Team
Your pulmonologist isn’t likely to talk to your cardiologist, gastroenterologist, or rheumatologist, so it’s up to you to update your care team if there are changes in your treatment plan. Making the most of your medical appointments can help make that team work for you and ensure you’re getting the best overall asthma care.
Here are some tips to know before you go:
- Be prepared with a quick summary of your conditions, especially if it’s a new doctor.
- Have ready a list of your health care providers and their contact info, plus a list of all your medications.
- Keep a diary of office visits and what the clinicians say.
- Always ask about drug interactions and contraindications.
- Bring your partner with you to help take notes.
- Ask lots of questions.
Getting Community Support
Living with multiple illnesses is a challenge. Just ask Carly. She says she has to take a more in-depth approach to her health and be very mindful. “What triggers my asthma can impact my lupus; a lupus flare can be triggered by stress. If my asthma is making me stressed, it can impact my lupus,” she says.
But Carly has strong community support through #LupusChat, an online hub for people with lupus and their caregivers, and the lupus community. The members talk about their symptoms and offer each other support and guidance.
The American Thoracic Society (ATS) has a forum to address the medical and social needs of the LGBTQ+ community. Dr. Michelle Harkins, MD, Professor and Chief of Pulmonary, Critical Care and Sleep at University of New Mexico, is part of the LGBTQ Allies and Interest Group at ATS. The organization is committed to bringing awareness to health issues and health disparities that may affect the LGBTQ+ population.
On a local level, Dr. Harkins runs the adult asthma clinic at the University of Albuquerque, where she serves a large LGBTQ+ patient base. “My mission there has been to invite the LGBTQ+ population into the clinic, address the comorbidities that go along with asthma, provide education to patients, and improve their asthma control.” Her greater mission has been to get equal care for LGBTQ+ patients and educate providers. “It can really help to be on the lookout for comorbidities and improve those aspects of care,” she says. “When you do, the asthma improves.”
Another place people with asthma and related conditions can find support is at No End in Sight Void or #NEISVoid. It is a hashtag that can be used to join Twitter conversations within the chronic illness community. Created in March 2020 by host Brianne Benness, the conversational space stresses no judgment and believing in people’s reported experiences. The host also has a podcast called No End in Sight.
Get Asthma Support
If you would like to receive emails about asthma support and education, please subscribe to the Global Healthy Living Foundation here.
This article was made possible with support from Amgen and AstraZeneca.
Althoff M, et al. Asthma and three colinear comorbidities: obesity, OSA and GERD. Journal of Allergy and Clinical Immunology in Practice. September 8, 2021. doi: https://doi.org/10.1016/j.jaip.2021.09.003.
Cazzola M, et al. Asthma and comorbidities: recent advances. Polish Archives of Internal Medicine. April 28, 2022. doi: https://doi.org/10.20452/pamw.16250.
Charoenngam N, et al. Patients with asthma have a higher risk of systemic lupus erythematosus: a systematic review and meta-analysis. Clinical Rheumatology. February 2021. doi: https://doi.org/https://doi.org/10.1007/s10067-020-05279-x.
Charoenngam N, et al. Patients with asthma have a higher risk of rheumatoid arthritis: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism. October 2020. doi: https://doi.org/10.1016/j.semarthrit.2020.07.015.
Interview with Dr. Michelle Harkins, MD, Professor and Chief of Pulmonary, Critical Care and Sleep at University of New Mexico.
Interview with Dr. Barbara P Yawn, MD, MSc, FAAFP, and Adjunct Professor at the University of Minnesota.
Miethe S, et al. Obesity and asthma. Journal of Allergy and Clinical Immunology. October 1, 2022. doi: https://doi.org/10.1016/j.jaci.2020.08.011.
Palmon P, et al. COVID-19 infections and asthma. Journal of Allergy and Clinical Immunology. March 2022. doi: https://doi.org/10.1016/j.jaip.2021.10.072.
If you enjoyed reading this article, you’ll love what our video has to offer.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo