BIPOC Patient Voices: Living with Psoriasis and Psoriatic Arthritis
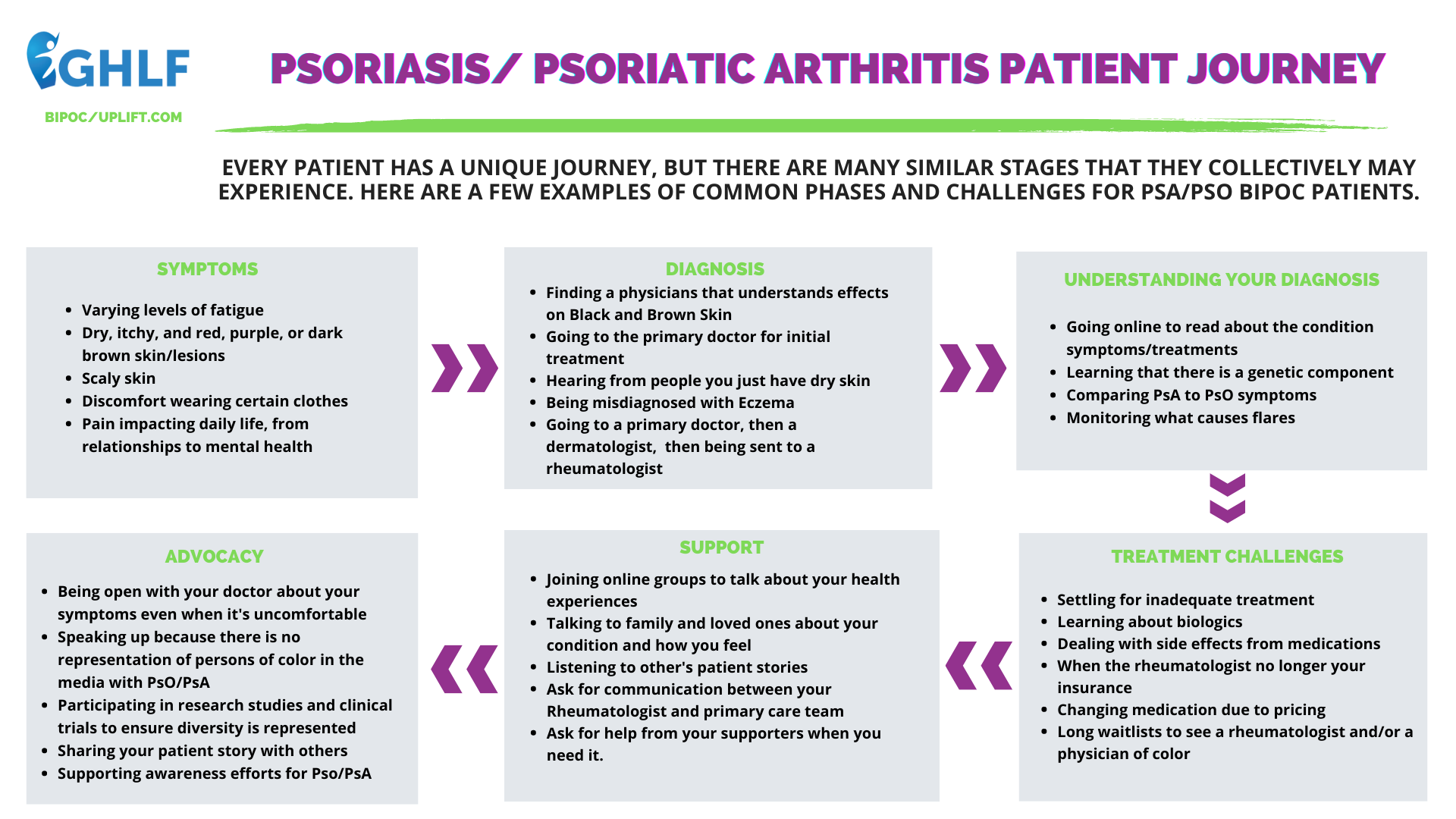
Managing a condition like psoriasis (PsO) or psoriatic arthritis (PsA) can be challenging — and perhaps even more challenging for Black, Indigenous, People of Color (BIPOC). The truth is that psoriasis and psoriatic arthritis do not discriminate — people of all races and ethnicities can experience these diseases — however everyone’s patient journey will not be the same.

By sharing the stories of BIPOC patients living with psoriasis and psoriatic arthritis, we’re hoping that others will listen to and learn from their disease journey. This conversation is vital for reducing health disparities and improving delays in diagnosis and access to treatment among patients in the BIPOC community. Representation matters in all aspects of life — and especially in health care.
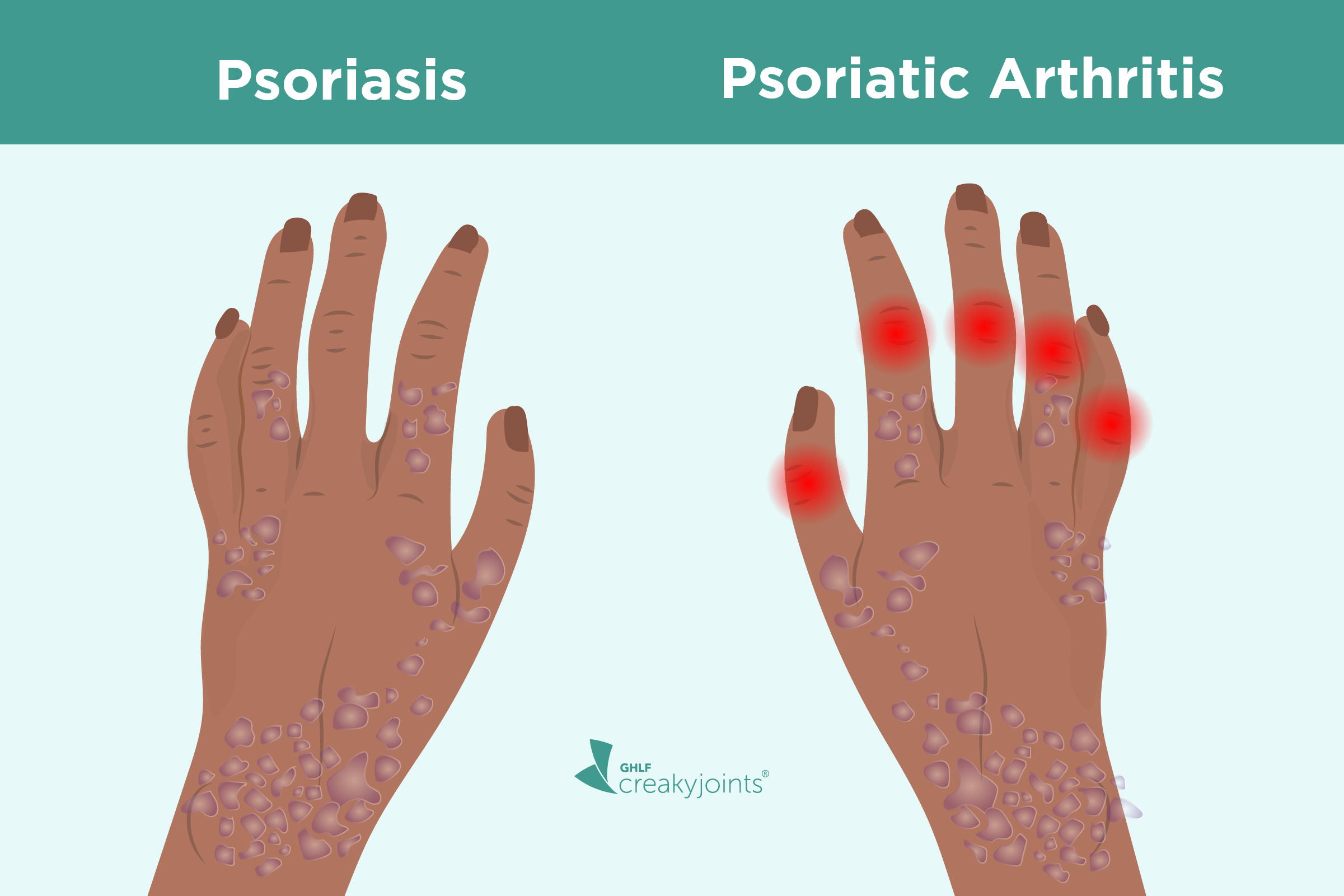
BIPOC patients, for example, often experience staggering delays in diagnosis as well as misdiagnosis and poor treatment when it comes to psoriatic disease as well as other chronic illnesses. In the case of psoriasis, this is partly due to a lack of knowledge about how the disease may present differently on different skin tones. The pink-to-red color typically seen with psoriasis on lighter skin often appears more purple or brown on darker skin tones. A lack of representation throughout media and within clinical trials may play a role. Without representation, BIPOC communities might not realize that their symptoms are related to psoriasis and psoriatic arthritis.
What Is Psoriasis and Psoriatic Arthritis?
Psoriasis and psoriatic arthritis are distinct conditions, but they are connected. Psoriasis is an inflammatory condition of the skin. At the same time, psoriatic arthritis also includes inflammation of the joints and etheses (places where a tendon or ligament attaches to the bone), called enthesitis. Psoriatic arthritis can complicate psoriasis, and is reported to occur in 7-26 percent of psoriasis sufferers.
Symptoms can vary from person to person depending on the type and severity of psoriasis or psoriatic arthritis. Psoriasis is most often associated with raised red, itchy, flaky skin patches, usually found on the knees and elbows. Psoriasis plaques may have a silver scale or crust on top, and some patients with psoriasis may notice thick, pitted fingernails. Those with fingernail changes are at higher risk for psoriatic arthritis. In skin of color, especially in deeper shades, the inflammation patches or scales can take a purplish brown color.
PsA is different than psoriasis alone in that it includes joint pain and swelling, and entheseal signs and symptoms. Patients with psoriasis and psoriatic arthritis often have other associated medical conditions, or comorbidities, such as metabolic syndrome, osteoporosis, or cardiovascular disease. Both the chronic inflammation of untreated psoriasis, and psoriasis risk factors, such as alcoholism and smoking, can increase the risk of early heart disease. Due to healthcare disparities and structural racism, BIPOC patients suffer disproportionately from both psoriasis risk factors and associated comorbidities.
Here’s a look into the BIPOC patient journey, including their struggles with finding the right doctor, getting a proper diagnosis and treatment, and coping with the stigma of living with a visible and often misunderstood chronic disease. Think about how this is different (or similar) to your health care journey.
Patient Perspectives: Navigating Care and More
We spoke with various BIPOC patients regarding their experience living with psoriatic disease and how it affects their daily life, including going to the doctor and engaging with their community. Research has long shown these health care disparities – delayed diagnosis and treatment, a lack of representation and culturally competent care, and the challenges accessing affordable, timely care. We spoke to patients to put a face to the facts. This video series features the perspective of other patients. This is not medical advice and should not take the place of professional medical care.
BIPOC Patient Voices: At Home with Psoriasis and Psoriatic Arthritis
BIPOC Patient Voices: In the Doctor’s Office with Psoriasis and Psoriatic Arthritis
BIPOC Patient Voices: In the Community with Psoriasis and Psoriatic Arthritis
Working with Your Care Team
PsO and PsA require regular care by a specialist, so finding the right rheumatologist and dermatologist is key to managing your condition. A rheumatologist is a doctor who treats conditions related to the bones, joints, muscles, and immune system. A dermatologist is a doctor who treats conditions related to the skin, nails, and hair.
The doctor-patient relationship has a significant impact on your well-being. It’s important to feel comfortable and safe to talk about what’s bothering you. This is your health, your life, and your future.
Health inequities exist and affect both the health care system and those trying to receive care and treatment. Having health care providers that can provide culturally competent care is essential in helping address disparities in health care.
Cultural competence in health care refers to the “ability of systems to provide care to patients with diverse values, beliefs and behaviors, including tailoring of health care delivery to meet patients’ social, cultural, and linguistic needs.” A lack of cultural competence in health care can have negative effects on patient safety such as “diagnostics errors, missed screenings, and harmful treatment interactions.”

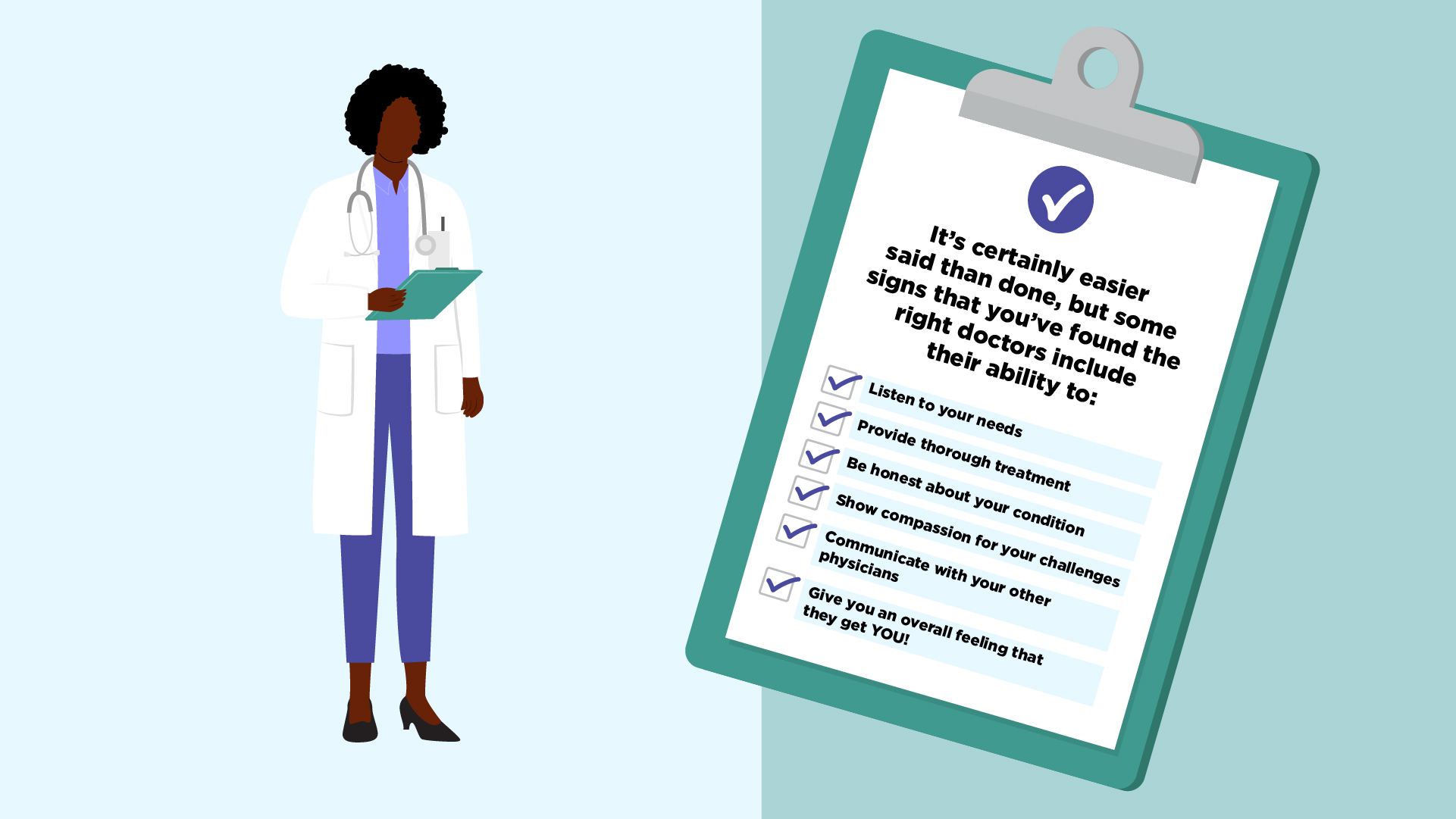
Unfortunately, finding a culturally competent physician can be a particular challenge for BIPOC patients. In the United States, BIPOC physicians are underrepresented with less than 5% of physicians self-reporting as Hispanic/Latinx or African American, and less than 1% reporting as Indigenous American.
An estimated 45 to 56 percent of people living with psoriasis also live with scalp psoriasis. Symptoms may include fine scaling that looks like dandruff, or thick, crusted plaques that cover the entire scalp. This can affect how people care for their hair. There may be cultural differences in hair care, or differences based on hair texture and styling. Black people, who are more likely to have traditionally stigmatized hair textures, may be particularly vulnerable to scalp disease-related distress. Further, the cadence and type of hair styling may vary by cultural background. It’s important that doctors be aware of this when recommending scalp and skin psoriasis treatments. This awareness may help in establishing a trusting therapeutic alliance between doctor and psoriasis patients.
Here are resources we recommend for BIPOC patients:
When you have psoriasis, you can get some pretty blunt, impolite questions and comments from people who don’t understand. The stigma of living with a skin condition can take its toll on your mental health.
Treating the emotional and mental symptoms of PsA or PsO are just as important as treating the physical ones. Battling mental health issues not only interferes with daily living, but it can lead to increased flares, pain, and fatigue; impact your work and relationships; and limit your ability to manage your overall health.
Managing your mental health will likely require a well-rounded approach that may include talk therapy, medication, and healthy lifestyle habits.
The Psoriatic Arthritis Club
You don’t have to manage psoriatic arthritis alone. This podcast can help.
Getting Clear on Psoriasis
A podcast series about what it takes to live better with psoriasis – from experts who treat it and patients who live with it
Get Involved in Advocacy
The 50-State Network is the grassroots advocacy arm of the Global Health Living Foundation and CreakyJoints. Through the 50-State Network, we train and help patients living with chronic illnesses to amplify their voice and add their personal perspective to health policy discussions. Join the 50-State Network to share your story about access to treatment, quality of care, and the need to prioritize the physician-patient relationship. Learn more and sign up here.


Get Involved in Research
Many studies on psoriatic disease have shown that the experience of having psoriatic disease in patients of color can be vastly different than white patients for a variety of socio-economic and cultural reasons. But there is still a lack of diversity in research, and a lack of research on the experience of psoriatic disease in BIPOC patients. Getting involved in research and sharing your experience helps impact future patients and ongoing treatment innovation.
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.

This project is produced by the non-profit Global Healthy Living Foundation, its arthritis patient community CreakyJoints, and made possible with support from Amgen.
Subscribe to CreakyJoints for more psoriatic disease resources
Medical Reviewer
Ashira Blazer
Dr. Ashira Blazer is an Assistant Professor of Rheumatology at Hospital for Special Surgery, who studies the biologic and genetic determinants of lupus severity in patients of African ancestry. She has forged multiple international collaborations with rheumatology programs in West Africa, spearheading the development of unique bio registries in Accra, Ghana, and Lagos, Nigeria. Dr. Blazer has received several funded grants through the Rheumatology Research Foundation, International League of Associations for Rheumatology (ILAR), Lupus Research Alliance, and the National Institutes of Health. She was most recently awarded a K23 research development award from NIAID to continue her work on APOL1 regulation and expression in lupus at HSS. Furthermore, Dr. Blazer is committed to mentorship and education and is working to advance diversity, equity, and inclusion in the field of Rheumatology in part through her role as the co-chair and inaugural member of the American College of Rheumatology DEI subcommittee. In recognition of her work as a thought leader in reducing health disparities, she was appointed as a 2020 National Minority Quality Forum 40 under 40 leader in Minority Health.

Alexis A, et al. Patients with psoriasis, skin of color experience disparities in identification, treatment. Healio. February 23, 2021. https://www.healio.com/news/dermatology/20210212/patients-with-psoriasis-skin-of-color-experience-disparities-in-identification-treatment.
Brach C, et al. Cultural Competence and Patient Safety. Agency for Healthcare Research and Quality. December 27, 2019. https://psnet.ahrq.gov/perspective/cultural-competence-and-patient-safety.
Creaky Staff. Psoriasis and Psoriatic Arthritis: What’s the Connection? CreakyJoints. October 02, 2020. https://creakyjoints.org/symptoms/psoriasis-and-psoriatic-arthritis-connection/.
Diversity in Medicine: Facts and Figures. Association of American Medical Colleges. 2018. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018.
Jara S. Psoriatic Arthritis and Mental Health: The Link to Depression, Anxiety, Fatigue and More. CreakyJoints. October 07, 2021. https://creakyjoints.org/about-arthritis/psoriatic-arthritis/psa-treatment/psoriatic-arthritis-mental-health/.
Prey S, et al. Assessment of risk of psoriatic arthritis in patients with plaque psoriasis: a systematic review of the literature. Journal of The European Academy of Dermatology and Venerology. April 24, 2010. doi: https://doi.org/10.1111/j.1468-3083.2009.03565.x
Scalp Psoriasis. National Psoriasis Foundation. https://www.psoriasis.org/scalp/.
Zickuhr L. Learn to recognize dermatologic changes in patients of color with rheumatic disease. ACR Convergence TODAY. November 05, 2021. https://www.acrconvergencetoday.org/learn-to-recognize-dermatologic-changes-in-patients-of-color-with-rheumatic-disease/.