In honor of World IBD Day, dietitians from three different continents share tips on managing diet and inflammatory bowel disease (IBD).
Joshua Denton’s Ulcerative Colitis Story: “I Didn’t Have a Lot of Exposure to What This Condition Was”
Joshua Denton’s Ulcerative Colitis Story: “I Didn’t Have a Lot of Exposure to What This Condition Was”
February 3, 2023
Kelsey Kloss

This story was told to the Global Healthy Living Foundation by Joshua Denton, a 37-year-old project manager in the aerospace industry who lives in Dallas, Texas. Joshua played football for the University of San Diego before opting out to manage his condition during his senior year of college. Today, he enjoys staying active by practicing yoga, playing intramural football, and lifting weights.
My journey with ulcerative colitis began my senior year of high school. I had what I would probably now consider to be relatively minor symptoms — such as abdominal pain and some discomfort during bowel movements. Less than a year later, I noticed a little bit of blood in my stool. That’s what catapulted me to disclose my symptoms to my parents.
What ensued after that would be a three-year journey. My family care physician wasn’t able to properly diagnose me at that time. I had bloodwork done and they did X-rays of my gastrointestinal tract. Originally, they diagnosed me as having a mild case of irritable bowel syndrome, or IBS for short. Then, they diagnosed me with lactose intolerance.
Only in 2007, after a colonoscopy, was I diagnosed with a mild case of ulcerative colitis — a type of inflammatory bowel disease (IBD).
Feeling Alone During My Diagnosis
During that time, I didn’t have much exposure to what this condition was. There wasn’t a lot of relatable data out there. Everything that was online at that time mostly corresponded with research that was being performed in the United Kingdom.
One of the interesting things was the notion that this was mostly (or almost exclusively) a Western European condition, in respect to the people who had it. Once I was diagnosed, I remember one of the first things I did was to Google ulcerative colitis and the people with it. I wanted to get a more ground-level understanding of where I fit within this experience.
It was very jarring: Most of the people they spoke about were all predominantly somewhere in Western Europe. There wasn’t a lot of documentation or valuable information for me to relate to, not just being Black — but even just being an American with this condition, because they considered it to affect such a small percentage of our population here.
There was an educational component to most of the conversations with family, friends, and even medical professionals. They were learning through my experience. It was pretty lonely, to be honest, and that part weighed on me a lot more than I acknowledged in the moment.
My Advice for Other Patients
For anyone who is newly diagnosed with this condition — and in particular, Black Americans — I would strongly encourage you to seek out some type of community. There are various online groups you can join. Some are directly tied to the condition and some may cover anything that is GI-related.
Having a space where you’re able to interact with other people navigating similar challenges goes a long way in gaining a healthy perspective on how to manage this condition. There’s obviously a physical component of how it affects your body, but when you’re dealing with a condition like this on a day-to-day basis, it wears on you mentally and emotionally as well.
Sometimes you need that support group to whom you can vent. With them, you don’t have to over-explain things because they understand the fundamentals of what you’re working through. You can focus on the nuanced aspects, which are very difficult to explain to someone who doesn’t have the condition or who is not caring for someone who has the condition.
Most importantly, if there are any local or regional organizations near you that have a physical space, I definitely encourage meeting up with those people. You benefit from having that one-to-one interaction. I only experienced that for the very first time in 2021 — and I didn’t meet anyone with my condition for the first 10 years.
How Far We’ve Come
Over the course of the past 17 years, we’ve made some notable strides in raising awareness around ulcerative colitis.
There are anecdotally a lot more people who may have at least heard of Crohn’s disease, even if they’re not directly familiar with ulcerative colitis. It helps when I’m trying to explain my condition that I’m able to say: “Well, hey, if you’re not familiar with ulcerative colitis, have you heard of Crohn’s?” Most people have heard of it, or are familiar with it. I explain that ulcerative colitis is basically a cousin or sibling of Crohn’s. It’s a similar condition, just in a separate part of your gastrointestinal tract.
From a medical community standpoint, significant strides have also been made. When I was initially diagnosed, not only was there no information, but there also weren’t any accommodations. The condition is now recognized as an official disability by the Americans with Disabilities Act, so when I’m applying for a job, I can disclose my condition upfront and be transparent. That allows for the company to provide accommodations I need.
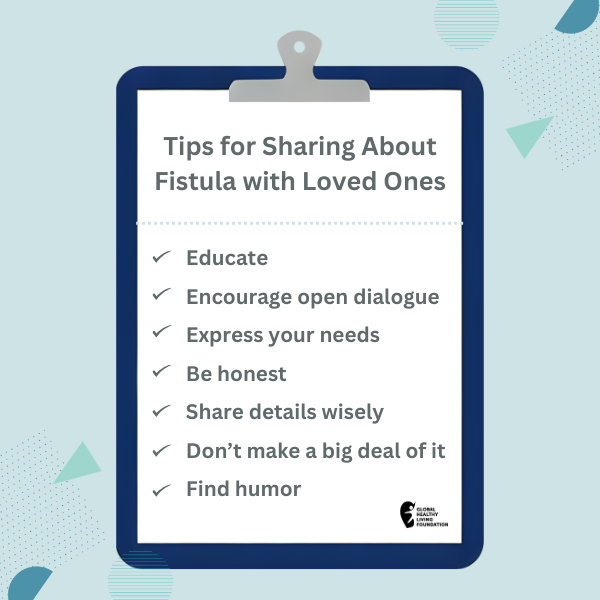
From a communication and awareness standpoint, it’s important to build a foundational level of support in those important places in your life — at home, at work, and around family and friends.
We now even have different pharmaceutical companies promoting drugs in commercials. Whether or not you use them, the passive benefit is that it raises awareness. The more explicit benefit is that it’s another option to manage a chronic condition that’s not technically curable.
Where We Can Go From Here
With the studies that have been done now, I think doctors are asking more questions and better questions on the front-end. That part is helping to establish or, in some cases, even restore trust between the patient and the medical health care professionals who are treating them.
Right now, in terms of overall awareness and the unfortunate growing nature of this disease, I think that general awareness has improved. When I was first diagnosed, there wasn’t a lot of data, information, or resources in this country. We’re probably now further along, but I don’t think things have fully matured.
I think we need a holistic approach to this condition and for the greater society to more fully grasp the nature of what it is. We’re starting to branch out to the relational experience of having ulcerative colitis. I may physically have it, but I was also married for a portion of my life and had this condition during my marriage. So it affects me on a day-to-day basis, but it would certainly impact my marriage and, by extension, my spouse as well.
If you have a child who’s diagnosed with this, it will also impact the parents and their ability to support their kid. That goes for everyone in between, too — including friends.
It’s difficult because it’s such a fluid situation: The symptoms are very unique and vary from one person to the next. There’s not a one-size-fits-all in terms of what it should look like and how it affects people. Being able to navigate the fluidity of this condition requires a holistic approach, because you don’t know how the condition is going to manifest in someone.
While we’ve made a lot of progress, I think that the ideal scenario would be to have the ability to talk about this outside of the medical community and outside of our immediate family and friends.
My Best Advice: Share Your Symptoms Now
I’ve dealt with this condition for nearly 20 years — and for at least three of those, I was not aware I had it. A huge reason why my diagnosis was delayed is because I didn’t even self-report. To some degree, I was afraid of the symptoms I was experiencing and what they meant.
Ignoring it, from a youthful standpoint, was very ignorant. I just thought that if I didn’t acknowledge it, eventually it’ll go away. Unfortunately, this is an autoimmune and chronic health condition and it’s not going anywhere. It’ll usually progress and get worse if left unattended.
The first thing I want to encourage folks to do: If you’re experiencing anything that is related to your digestive tract and it seems out of the norm, err on the side of caution and go get it checked out. I understand the fear and I genuinely understand where it comes from. But again, ignoring it is not going to solve it.
The second thing I would say is, if you’re diagnosed, don’t let that fear prevent you from being transparent and advocating for yourself. Advocating can look a lot of different ways, but I think at the very least it begins with you being able to advocate for yourself in the doctor’s office.
When needed, it can also expand to your place of work or where you reside. We need to make sure that in each individual place, we’re very comfortable talking about something that’s a very taboo topic in many respects, culturally and individually.
Once we’re able to get to a place of sharing what our experience looks like and being transparent, it allows us to build connections with those who may not experience it — but who are empathetic and want to understand.
They can only understand if we give them the opportunity to, and that begins with us sharing our experience and our stories, staying consistent, and being transparent.
Want to Get More Involved with Patient Advocacy?
Your voice in advocacy matters. The 50-State Network is the grassroots advocacy arm of CreakyJoints and the Global Healthy Living Foundation, comprised of patients with chronic illness who are trained as health care activists to proactively connect with local, state, and federal health policy stakeholders to share their perspective and influence change. If you want to effect change and make health care more affordable and accessible to patients with chronic illness, learn more here.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo