In honor of World IBD Day, dietitians from three different continents share tips on managing diet and inflammatory bowel disease (IBD).
Crohn’s and Fistula: Coping with the Emotions of Another Diagnosis
Crohn’s and Fistula: Coping with the Emotions of Another Diagnosis
January 26, 2023
Barbara Brody

Check out Your Guide to Understanding Complex Perianal Fistula for more information on this topic.
About 10 years ago, Tina Aswani-Omprakash was throwing up in the bathroom during a wedding when she realized that she had a new and serious problem. “I was 40 pounds heavier thanks to taking prednisone [to control a Crohn’s disease flare] and generally feeling like crap when I realized something was hurting down there,” recalls Aswani-Omprakash, patient advocate of the blog Own Your Crohn’s and President of the nonprofit charity South Asian IBD Alliance (SAIA).
She felt around and found that she had something resembling a boil in her vagina. “I saw mucus and blood and some feces and thought, ‘Oh wait, it’s not supposed to come from there. What is my body doing to me?’”
For patient advocate and SAIA’s Project Manage Chaitanya Kiran Pullela, who lives in India, the fistulas started before he even knew that he had Crohn’s. “I was in college, and I was having painful abscesses that would drench my underwear and pants,” he says. “I went to a surgeon, but no one told me that it was Crohn’s” until several years later.
About 25 percent of Crohn’s disease patients develop perianal fistulas. This somewhat common complication is notoriously difficult to treat, and many people end up requiring several surgeries in addition to medication such as antibiotics and biologics, says Stefan D. Holubar, MD, IBD Surgery Section Chief and Director of Research in the Department of Colon & Rectal Surgery at the Cleveland Clinic.
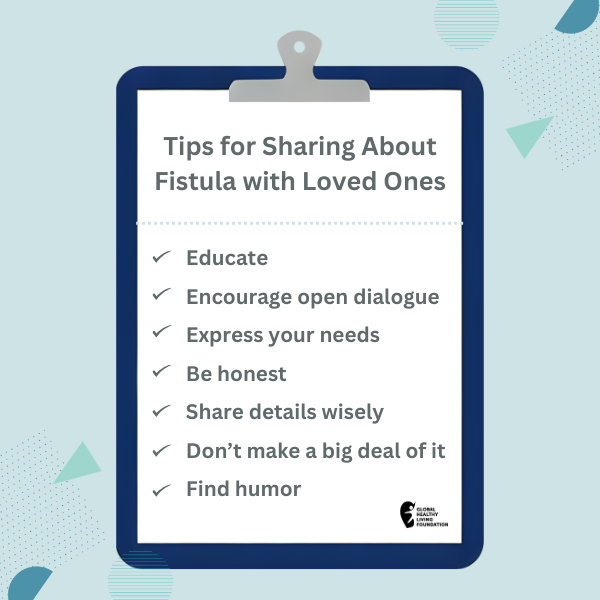
Patients are typically reluctant to discuss what they perceive as an embarrassing or intimate problem. This desire for privacy, while understandable, has the potential to further compound feelings of isolation and distress. In many cases, patients cycle through a rollercoaster of emotions as they contend with having a new diagnosis on top of their Crohn’s disease.
The Emotional Toll of Living With Fistulas
Finding out that you have a fistula can be pretty frightening, especially if you don’t understand what’s happening or why.
“It’s really scary and violating,” says Aswani-Omprakash. “It’s one thing to be bleeding because of Crohn’s disease or ulcerative colitis, but it’s another to see holes and have draining come out of weird parts of your body. I remember thinking, ‘Can my body stop betraying me?’”
Embarrassment
Embarrassment is also common, says Michele Rubin, APRN, an IBD Clinical Nurse Specialist in the University of Chicago Medical Center. She often sees young teens who have five or six fistulas draining and need medical treatment as well as mental health care. “These kids are basement dwellers who are so embarrassed they barely look at you in the clinic,” she says. “They don’t want to say anything, and some of them don’t even want you to look at their butt” despite the fact that an exam is necessary for proper diagnosis and treatment.
Hope and Relief
Some patients do experience moments of hope and relief, especially when they first learn that their problem has a name and that treatment options exist. But any positivity tends to be dashed once they learn that there’s no quick fix and that even surgery may not completely resolve the problem, says Dr. Holubar.
Frustration
Others become exhausted and frustrated because of how difficult it is to get the right help. It took about four years for Pullela to get a Crohn’s diagnosis after he first started developing fistulas; he now travels about 300 miles — the equivalent of going from NYC to Boston — in order to see a doctor who has the right expertise.
Even in the U.S., good care isn’t guaranteed. There are only about 2,500 colorectal surgeons in the entire country, says Dr. Holubar, and other medical providers don’t always have the right tools and knowledge to properly address fistulas and Crohn’s disease.
“Some primary care doctors don’t even know to refer a patient out to a gastroenterologist” when they develop a fistula, says Aswani-Omprakash. She recalls meeting a woman at a support group who was repeatedly going to a general surgeon to have a fistula drained yet was never directed to an inflammatory bowel disease (IBD) specialist.
How to Cope With the Emotional Aspects of Fistulas
Living with severe Crohn’s disease and complications such as a complex perianal fistula comes with an array of challenges that can chip away at your self-esteem and lead to stress, depression, and anxiety, but there is reason to be hopeful.
Starting treatment as early as possible can pave the way for better quality of life, says Rubin. At the same time, you can take steps to bolster your emotional well-being.
Educate yourself
Knowledge really is power as well as the key to dispelling fear about the unknown. Ask your gastroenterologist or colorectal surgeon as many questions as needed, and learn about the condition and treatment options from trusted sources.
“Seek out information from the right people,” says Rubin, who recommends going to the website of the Crohn’s & Colitis Foundation. The organization also runs a chat service you can access online or contact via phone (888-694-8872, extension 8).
Find the right providers
If at all possible, get yourself to an IBD center of excellence — a specialized IBD program housed at a major medical institution — advises Rubin. At the very least, make sure you find a provider who treats a lot of patients with fistulas. The right provider should certainly be able to provide excellent medical care, but you also want someone who empowers you to take an active part in your treatment.
“It’s important that there is shared decision-making between patient and provider,” says Rubin. Communication from both parties is key. Your provider should explain what’s happening and help you set realistic goals for your treatment while at the same time taking your feedback seriously.
Mental health treatment is also crucial. A health psychologist — ideally, someone who specializes in gastropsychology — can help you work through any depression or anxiety you may be feeling as a result of your health problems. Ask your doctor if they can refer you to an appropriate therapist, or visit romegipsych.org/ to search for a gastropsychologist in your area.
If local resources don’t exist, consider exploring virtual help, such as online IBD resiliency training through Trellus Health. This program was developed by leaders in positive psychology, including Co-Founder Laurie Keefer, PhD, Director of Psychobehavioral Research, Division of Gastroenterology, at Icahn School of Medicine at Mount Sinai.
Seek out extra support
Aswani-Omprakash’s mother sent her to an IBD support group soon after she had her first surgery, and she’s glad that she was given the push. “In the beginning, I would never talk; I was just taking it in,” she says. Today, she is an outspoken advocate who helps run an online support group. “You have to start somewhere, and it really helps to make friends in [the IBD] community,” she says.
Keep in mind that the first support group you try may or may not be a good fit, says Keefer. “Fistulizing perianal disease is kind of under-supported in the IBD world,” she says. She recommends searching for groups (online or in your area) that specifically cater to people with fistulas.
Embrace and accept it
Living with Crohn’s disease and fistulas is clearly difficult, but it’s best to accept your reality since it really can’t be ignored, says Keefer, who encourages patients to practice self-compassion. “This is something you have to give your time and attention to. Even when you’re feeling OK, it’s still like a background app that’s always tracking your location. The more you try to avoid it, the more energy you spend on it,” she says.
Aim for optimism
That doesn’t mean viewing everything through rose-colored glasses. But Keefer advises patients to remember that their disease isn’t the only important thing about them. You may also be a spouse, friend, employee, artist, and so on. She also reminds them that their situation is not permanent, as new treatments, such as new drugs that specifically target fistula and stem cell therapy that is already being used in other countries. Clinical trials are ongoing in the U.S. right now.
Gut Culture Podcast
Check out Gut Culture, a podcast that gut checks assumptions about IBD (Inflammatory Bowel Disease) through real conversations with two health care leaders. Listen now.
This article was made possible with support from Takeda and Bristol Myers Squibb.
Gao X, et al. “Symptoms of Anxiety/Depression Is Associated with More Aggressive Inflammatory Bowel Disease.” Scientific Reports 11. January 14, 2021. doi: https://doi.org/10.1038/s41598-021-81213-8.
Interview with Laurie Keefer, PhD, Director of Psychobehavioral Research, Division of Gastroenterology, at Icahn School of Medicine at Mount Sinai
Interview with Michele Rubin, APRN, an IBD clinical nurse specialist in the University of Chicago Medical Center.
Interview Stefan D. Holubar, MD, IBD Surgery Section Chief and Director of Research in the Department of Colon & Rectal Surgery at the Cleveland Clinic.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo