Take charge of your asthma and associated conditions. Get tips on teaming up with specialists and confidently advocating for your care.
Understanding Barriers to Asthma Treatment
Understanding Barriers to Asthma Treatment
Accessing the right asthma treatment isn’t always easy. Here, we explore some barriers and offer tips to help enhance your asthma care.
September 19, 2023
Nina Wasserman

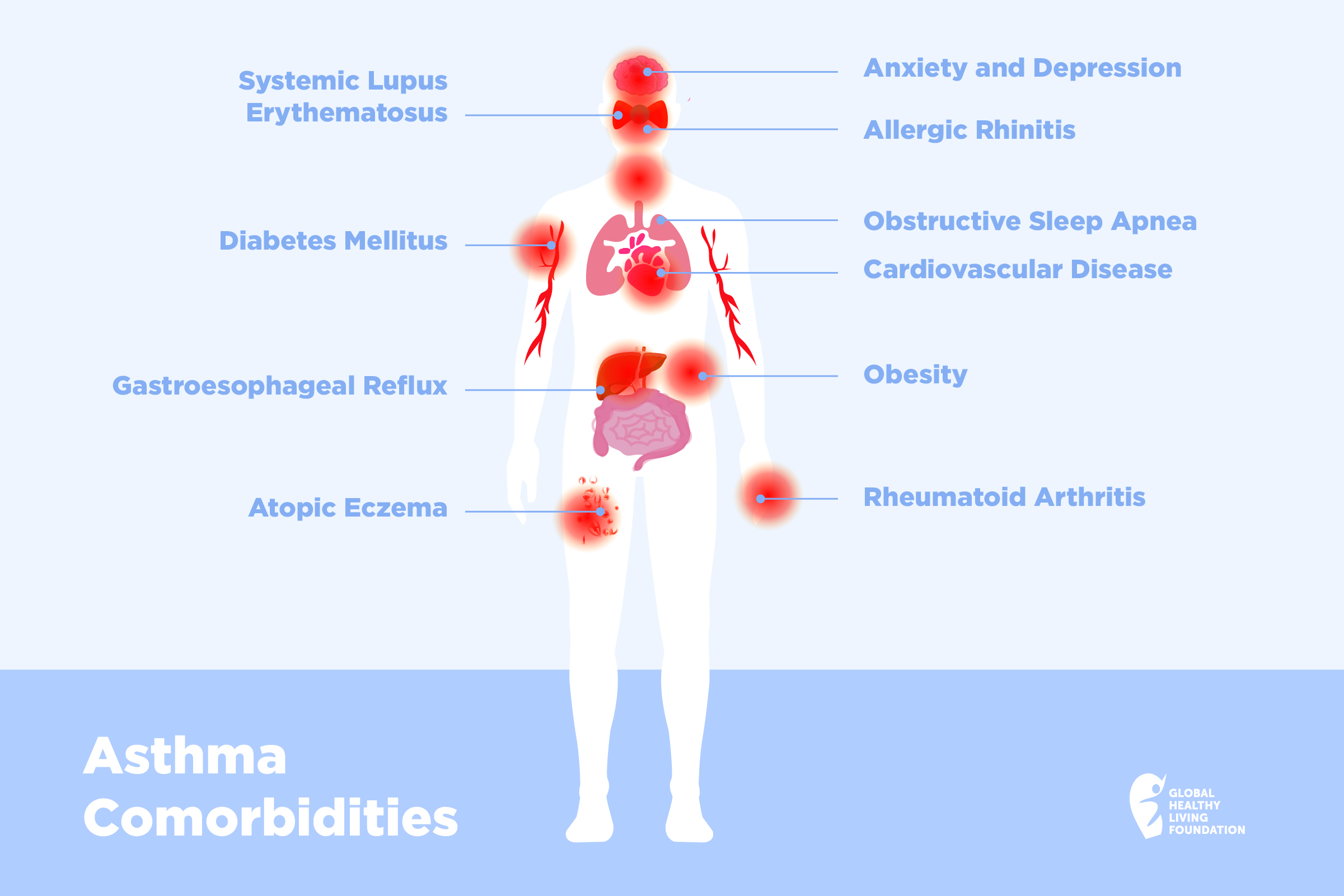
Nearly 26 million people in the U.S. have asthma, most notably adults ages 35 to 64. The reassuring part is that asthma can be controlled both by medication and by avoiding the triggers that cause your asthma.
However, data from the Centers for Disease Control and Prevention statistics, updated in 2022, indicates that about 60 percent of adults with asthma don’t have it fully under control. Uncontrolled asthma can lead to more severe flare-ups, increased emergency room visits, hospital stays, and missed workdays.
There are multiple reasons why asthma remains uncontrolled for many. It’s crucial to understand these challenges to seek the best possible care.
Lack of Access and Fragmented Care
To start your asthma treatment journey, it’s essential to see a doctor. According to Dr. Barbara Yawn, MD, MSc, FAAFP, an Adjunct Professor at the University of Minnesota, most asthma patients receive care from a primary care doctor. However, not everyone has access to a primary care physician, where consistent and collaborative health management, or continuity of care, is offered.
In some parts of the country, primary care physicians are readily available, but many other areas face a shortage. “It can be problematic to get a visit with a primary care clinician in some areas, with extensive waits for appointments,” says Dr. Yawn.
But there’s another facet to consider: timely follow-up care. Dr. Yawn emphasizes that asthma treatment isn’t just about addressing urgent issues. It’s crucial to proactively prevent flare-ups through regular asthma check-ups, she notes.
Moreover, Dr. Yawn points out the rise of storefront clinics and urgent care centers. “While people may have easy access to those places, they are problematic because the care is fragmented. You cannot manage a chronic disease by getting bits of care here and there. People with asthma need chronic disease management.”
Cost of Care
Another barrier to treatment is cost. Roughly 27 million Americans lack health insurance, and even among those insured, many face limited coverage or steep deductibles.
While concerns about expenses might deter someone from visiting a doctor, neglecting one’s health can often lead to even greater costs in the long run.
Disparities in Care
Under-resourced communities experience a disproportionate impact from asthma, notes Lynda Mitchell, CEO of the Allergy & Asthma Network. Black, Hispanic/Latino, and Native Americans often have increased rates of emergency department visits and deaths due to asthma.
“Ongoing disparities in care impact asthma treatment,” says Mitchell.
Reasons for these disparities include:
- Proximity to highways, leading to more exposure to air pollution
- Housing challenges in certain urban areas with greater exposure to asthma triggers like mold, dust mites, cockroaches, and mice
- Lower income levels
- A shortage of asthma specialists or health care resources in marginalized communities
- Restricted or no access to transportation for medical visits
- Communication barriers, including language or cultural differences, that can hinder understanding of treatment or proper inhaler use
Getting a Specialist
For individuals with asthma, sometimes a specialist — like an allergist or pulmonologist — is essential to identify triggers and prescribe appropriate medications. However, securing these specialist appointments isn’t always straightforward.
Maya G. initially consulted a primary care physician. However, due to her combination of asthma, allergies, and long-COVID symptoms, she expanded her care team to include a pulmonologist, allergist, and an ENT (ear, nose, and throat) specialist. “Getting in to see my pulmonologist is a real challenge,” Maya adds. “It’s a constant process of advocating for myself to get the care I need.”
Specialists are usually best equipped to manage severe or uncontrolled asthma and are often more informed about the latest treatments. However, accessing them can be a challenge, potentially hindering patients from collaborative decision-making and optimal care, notes Mitchell.
Here are some common challenges in accessing specialty care:
Specialty Visit Restrictions
Many insurance plans cap the number of specialist visits or charge higher co-pays for them. Additionally, some policies mandate a primary care consultation before seeing a specialist, increasing treatment costs.
Referral Requirements
Some patients must first obtain a referral from their primary care doctor. This extra step can postpone vital treatment. If you arrive at a specialist’s clinic without the necessary referral, you might need to reschedule.
Geographical Barriers
People in rural areas may have to travel long distances to see a specialist. Yet there are also obstacles in urban areas like lack of transportation or extensive commutes via public transit.
Appointment Availability
Sometimes getting an appointment with a specialist can take up to a month or more. These delays can lead to disease progression or complications.
One way to increase your access to specialists is to do a little homework. To enhance your access to specialists, it’s beneficial to do some research. Review your insurance plan to find in-network specialists. While your primary care doctor might refer you to an out-of-network professional, consider telehealth visits as an alternative when in-person consultations are challenging.
High Out-of-Pocket Costs
According to a recent study published by the CDC on the individual medical costs for asthma, the annual per-person medical cost stands at $3,266. Of this, prescriptions account for the largest portion, totaling $1,830.
Inhalers constitute the majority of this prescription expense. Despite being in use for nearly 65 years, there are very few generic options available. A report from the Centers for Medicaid and Medicare Services, found that seven of the 50 most costly drugs for Medicare are brand-name inhalers.
“Patients don’t often think about bringing up prescription costs with their doctor, so the topic often goes undiscussed at appointments,” says Mitchell. She says doctors should be prepared to bring up and discuss out-of-pocket expenses as a factor in a patient’s overall care plan. They can suggest generic inhalers that are, in most cases, less expensive. They may be able to pass on product samples or drug discounts.
The Asthma and Allergy Network has a summary of inhaler discount programs.
If You Can’t Afford Your Asthma Medication
There are some simple steps you can take to help bring down your medication costs. According to the Allergy and Asthma Network you can:
Check Your Plan
Visit online to find out which medications are under your plan. The insurance drug list — called a formulary — should be found on your insurance company’s website. To find out how to read a formulary read this article or you can watch this webinar. You will need to check once or twice a year since the covered medications can change frequently, especially for common medications like asthma inhalers.
Shop Around
Check your medication price at other pharmacies or online options such as GoodRx, Singlecare, Needymeds, and Amazon Pharmacy.
Ask for Generics
Even if your prescription is for a brand-name drug, you can ask your pharmacist for a generic version, if there is one. There are some membership-based online plans that offer generic drugs such as Costco and MarkCuban CostPlus Drug Company. Amazon prime members can get generic drugs for a flat fee of $5 a month through the Amazon Prime RxPass.
Call the Manufacturer
Some drug companies have patient assistance programs that you may be eligible for. You can find information about these programs online.
Discuss Alternatives with Your Doctor
There may be an effective replacement medication at a cheaper price. It never hurts to ask.
Find Help with Out-of-Pocket Costs
There are programs that can help you pay your deductible using tax free dollars. Find out more here.
“From an advocacy perspective, a few states have passed laws that put caps on the price of asthma inhalers,” says Mitchell. “This would reduce the cost barriers that prevent many lower-income families from getting the medications they need. Similar legislation should be enacted on the federal level. Making asthma inhalers more affordable helps ensure these potentially life-saving medications are more readily available.”
Step Therapy and Asthma Treatment
Step therapy is a process in which health insurers aim to control costs. The insurer will require the patient to fail the first step of treatment before moving on to a second step, even though the doctor and patient may have agreed step two is the best treatment option, says Mitchell.
The first step is often a generic or low-cost medication. Step two is often a more expensive medication for the insurer to cover. The approach can work well for the majority who benefit from the first step of medications, but it can be a barrier for those with more severe asthma.
“This compromises patient treatment and it can actually lead to increased costs for both the patient and the insurance company in the long term,” says Mitchell.
Patients who are in step therapy should talk with their doctor. The doctor may be able to appeal the health insurer’s decision on your behalf, says Mitchell.
If access to the best medication has been delayed for you, here are some ways you can advocate for the stepped-up treatment you need:
- Keep track of the medications, amounts, how long you have taken them, how well your asthma was controlled and any changes in your symptoms.
- Let your doctor know immediately if there is a worsening of your symptoms, or if you have to visit an emergency department or urgent care center because of an asthma attack.
- Find a convenient time to make calls to your insurance company, as they can have wait times that last more than an hour.
- Be patient, but assertive when on the phone with the insurance company.
- Don’t give up — being your own patient advocate produces results.
Prior Authorization for Asthma Medication
Prior authorization is a tool used by insurance companies to make sure a patient is getting the right and necessary help for their health. You may need prior authorizations for medicine, specialist visits, testing, or imaging. If a medication needs prior authorization, your doctor will have to provide evidence to the insurance company from your patient records to prove that it is necessary.
The problem with prior authorization is that the time it takes your physician to provide the appropriate information to your insurance company for their approval is time that is delaying your treatment. And then if the authorization is denied, where does that leave you? You have to return to your doctor and find another way.
“This can be a real frustration,” says Dr. Yawn. It is important to remember that the idea behind prior authorization is to keep medical costs down and avoid overprescribing medication.
What should you do if your medication needs prior authorization? Take these steps to help the process go smoother so you can get the right treatment as soon as possible:
- Plan ahead. If you know you are going to need prior authorization for a medication, plan ahead and let your doctor’s office know so the paperwork can be ready.
- Stay on top of repeat prescriptions. If this is a prescription that requires repeated authorizations for renewals, get ahead of the game by informing your doctor before your current prescription runs out.
- Switch medications. Ask your doctor if there is any other effective substitute that does not require prior authorization.
- Stay organized. If a certain letter or test result worked once to get approval, keep it in your own files to use again.
Mitchell notes that more than 30 states are developing legislation to establish quicker response times under prior authorization and prohibit retroactive denials. Legislation in Congress is also underway to create a more standardized electronic prior authorization system.
Quantity Limits
Quantity limits are limitations set by insurance companies on how much of a certain treatment you can receive over a specific period of time period. There are good reasons for quantity limits. They are put in place to protect patients from overuse. For example, national guidelines recommend a “rule of two” for rescue inhalers, meaning you should be using your rescue inhaler twice or less per week. The reason for this is that too much albuterol can be harmful.
However, quantity limits can pose a barrier to treatment. For example, if there are limits on devices such as inhalers, what happens if your device is broken or lost? Or what if you need inhalers in multiple places for emergencies, such as a child might need an inhaler at home, at school and at their after-care location?
But Dr. Yawn says your pharmacist or clinician can help you make an appeal to your insurance company for additional devices. Another option is to go through mail order medications where it might be possible to get multiple devices.
Non-Adherence to Asthma Treatment Plan
A final barrier to getting treatment for asthma is when a patient does not follow the treatment plan they and their doctor agreed upon. Medication, follow-up visits, procedures and lifestyle changes are all areas where a patient can make the difference between complying or not.
A 2022 study published in the Cochrane Database of Systematic Reviews reported a 45 percent asthma medication adherence rate for patients who had no interventions other than just a visit. That means that over half of the people with asthma were not getting any or enough of their medications.
Patients have many reasons for not using their asthma medications. According to a study published in BMC Pulmonary Medicine, the reasons may include:
- Fear of adverse effects
- Fear of medication dependence or addiction
- Distrust that medication is effective or necessary
- Concern that medication will stop working
- Preference for alternative treatment
- Inconvenient dosage regimens
- Cost
- Stigmatization
- Lack of social support
It’s not easy to start a new treatment regimen that you feel unsure about. And many patients have low expectations — they don’t feel like their asthma is going to get better, so they just accept it.
But non-adherence to medication can come at a cost. You may suffer preventable asthma symptoms of breathlessness, wheezing, and tightness in your chest. There is also a tendency to rely and overuse your rescue inhaler and not take the daily maintenance medicine, which can lead to more serious symptoms.
If your asthma remains uncontrolled, it will affect your work, family, well-being, and long-term health.
To avoid exacerbating your asthma attacks and to get your breathing under control, Dr. Yawn suggests using multiple tools to help you remember your daily routine, whether it’s taking your medicines once or twice a day.
- Put your inhalers in plain sight in the bathroom or by the kitchen sink — wherever you will see it in the morning and before bed
- Use your cellphone to notify you with reminders of when to take your medicine
- If you are uncomfortable with your phone, ask your kids to put reminders on their phones
If you are reluctant to take your medicine, ask yourself why, says Dr. Yawn. Is it because you think you feel, okay? Just because you feel good today, doesn’t mean your asthma won’t be worse tomorrow. And if you have fears or concerns, talk to your doctor or nurse to get more information.
The best way to manage a chronic condition is to be consistent and take your medication as you and your doctor have agreed upon.
Get Asthma Support
If you would like to receive emails about asthma support and education, please subscribe to the Global Healthy Living Foundation here.
This article was made possible with support from Amgen and AstraZeneca.
Chan A, et al. Digital interventions to improve adherence to maintenance medication in asthma. Cochrane Database System Review. June 2022. doi: https://doi.org/10.1002/14651858.CD013030.pub2.
Interview with Lynda Mitchell, CEO of Allergy & Asthma Network.
Interview with Dr. Barbara P Yawn, MD, MSc, FAAFP, and Adjunct Professor at the University of Minnesota.
Nurmagambetov T, et al. The economic burden of asthma in the United States. Annals of the American Thoracic Society. 2017. https://www.thoracic.org/about/newsroom/press-releases/resources/asthma-costs-in-us.pdf.
Pelaez S, et al. Patients’ perspective of barriers and facilitators to taking long-term controller medication for asthma: a novel taxonomy. BMC Pulmonary Medicine. April 2015. https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-015-0044-9#Sec1.
If you enjoyed reading this article, you’ll love what our video has to offer.
SUBSCRIBE TO GHLF
RELATED POST AND PAGES
_
Was this article helpful?
YesNo